Key Takeaways
- Eye swelling is a normal response after most ocular procedures, usually peaking within 24‑48 hours.
- Typical swelling subsides in 3‑7 days; lingering redness or pain may signal infection.
- Cold compresses, head elevation, and prescribed eye drops are the most effective home‑care tools.
- Know the red‑flag signs-intense pain, vision loss, or spreading warmth-that require immediate ophthalmologist attention.
- Staying hydrated, avoiding rubbing, and protecting your eyes from bright light speed up recovery.
When you notice eye swelling after surgery is a common postoperative response that can feel alarming, it helps to understand what’s really happening inside the eye socket. This guide walks you through the causes, the typical timeline, warning signs, and practical steps to keep the swelling under control so you can get back to clear vision faster.
What Is Eye Swelling After Surgery?
Postoperative edema is swelling that occurs after an operation as blood vessels leak fluid into surrounding tissues. In the eye, that fluid builds up in the conjunctiva, eyelids, and sometimes the orbital fat, creating the puffiness most patients notice. The swelling is part of the body’s natural healing cascade-blood vessels expand, inflammatory cells arrive, and extra fluid cushions the delicate structures while they repair.
Why Does It Happen?
Several mechanisms drive the puffiness:
- Trauma to tiny blood vessels during the procedure releases inflammatory mediators.
- Manipulation of the eye during cataract surgery can irritate the conjunctiva and cause temporary leakage.
- Laser‑based corrections such as LASIK create a micro‑vacuum that triggers a brief inflammatory response.
- Use of intra‑ocular devices or sutures can provoke a mild foreign‑body reaction, adding to fluid buildup.
Most of these reactions are harmless and resolve on their own, but they set the stage for the swelling you’ll see.
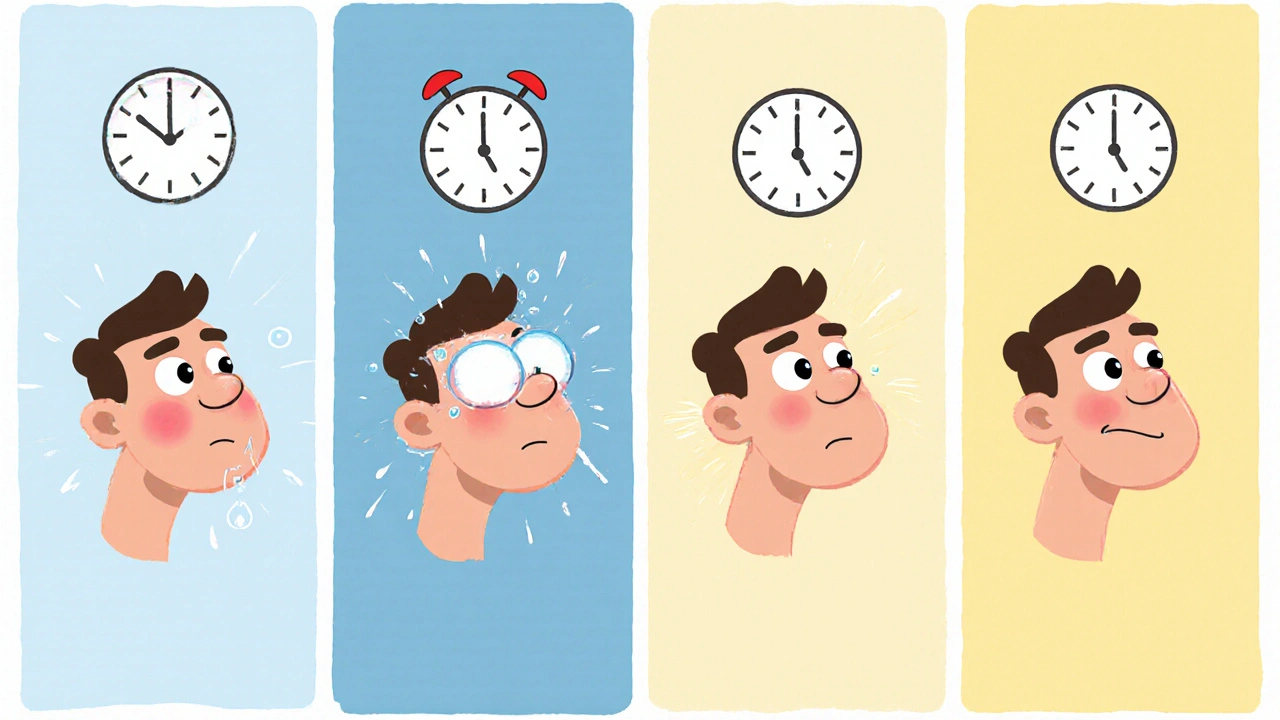
Typical Timeline - When Will It Calm Down?
Understanding the usual course helps keep anxiety in check:
- 0‑12 hours: Mild bruising and a thin layer of fluid appear.
- 12‑48 hours: Swelling peaks; eyelids may feel tight and eyes look glossy.
- 3‑5 days: Most fluid is reabsorbed. Discomfort drops dramatically.
- 7‑10 days: Residual puffiness fades; vision is usually stable.
If swelling persists beyond two weeks or worsens, it’s time to call your eye doctor.
Red‑Flag Symptoms - When to Seek Immediate Help
While most swelling is benign, certain signs point to complications like infection or orbital cellulitis, a serious bacterial infection of the eye socket. Contact your ophthalmologist immediately if you notice:
- Severe throbbing pain that doesn’t improve with over‑the‑counter pain relievers.
- Rapid spreading redness or warmth extending beyond the eyelid.
- Vision blurring, double vision, or sudden loss of sight.
- Fever over 38 °C (100.4 °F) accompanied by chills.
These symptoms could indicate an infection that needs antibiotics or, in rare cases, surgical drainage.
Home‑Care Strategies That Actually Work
Most patients find relief with a combination of simple measures. Below is a quick‑reference table that compares the most common approaches.
| Method | How It Works | Typical Duration | Effectiveness |
|---|---|---|---|
| Cold compress | Constricts blood vessels, reduces fluid leakage | 10‑15 min, repeat every 2‑3 h | High |
| Head elevation (sleeping on extra pillows) | Gravity helps drain excess fluid | All night, especially first 3 days | Medium |
| Anti‑inflammatory eye drops | Blocks prostaglandin pathways, lessens inflammation | Prescribed course, usually 5‑7 days | High |
| Hydration & balanced diet | Supports overall fluid balance, reduces congestion | Continuous | Medium |
| Avoid rubbing & screen glare | Prevents mechanical irritation and further inflammation | First week | Medium |
Here’s how to apply each method safely:
- Cold compress: Wrap a clean gel pack or a bag of frozen peas in a thin towel. Press gently over the closed eyelid for 10‑15 minutes, then remove for at least 20 minutes. Repeat as needed, but never apply ice directly to the skin.
- Head elevation: Use two or three extra pillows to keep your head higher than your heart while you sleep. This simple trick can cut swelling by 30‑40 % in the first days.
- Anti‑inflammatory eye drops: Your surgeon may prescribe ketorolac or a similar non‑steroidal anti‑inflammatory drug (NSAID) eye drop. Follow the dosing schedule exactly; missing doses can prolong inflammation.
- Hydration: Aim for at least 2‑3 liters of water daily. Dehydration makes the body retain fluid, paradoxically worsening puffiness.
- Avoid rubbing: Even a gentle rub can reopen tiny blood vessels. If your eye feels itchy, use a cool, damp washcloth instead of your fingers.

Medical Interventions: When Prescription Matters
Beyond the home measures, doctors may add one or more of the following based on your specific procedure:
- Steroid eye drops (e.g., prednisolone acetate) reduce severe inflammation when NSAID drops aren’t enough.
- Oral anti‑inflammatory medication such as ibuprofen can complement topical therapy for more extensive swelling.
- If infection is suspected, antibiotic eye drops or oral antibiotics may be prescribed.
- In rare cases of persistent fluid, a minor procedural aspiration performed by the ophthalmologist can evacuate excess fluid.
Never self‑prescribe steroids-they can raise intra‑ocular pressure and jeopardize recovery.
Lifestyle Tips to Speed Up Healing
Small daily habits make a big difference:
- Wear sunglasses outdoors for the first week to shield the healing eye from UV light and wind.
- Limit screen time; the blue light can dry out the eye and increase discomfort.
- Consume foods rich in omega‑3 fatty acids (salmon, walnuts) which have natural anti‑inflammatory properties.
- Practice gentle eye exercises only if your surgeon approves; excessive movement can aggravate swelling.
- Schedule a follow‑up visit as instructed-usually within 24‑48 hours-to ensure the eye is healing properly.
Frequently Asked Questions
How long should I use cold compresses?
Apply a cold compress for 10‑15 minutes, then rest for at least 20 minutes. Repeat every 2‑3 hours during the first 48 hours. After that, reduce frequency as swelling improves.
Can I wear contact lenses while my eye is swollen?
Generally no. Contacts can trap bacteria and irritate the already inflamed tissue. Switch to glasses until the swelling resolves and your doctor clears you for contacts.
Is swelling a sign of a serious complication?
Mild to moderate swelling is normal. Severe pain, fever, vision loss, or spreading redness are warning signs that require immediate medical attention.
Should I take over‑the‑counter pain relievers?
Acetaminophen or ibuprofen can help with discomfort and also reduce inflammation. Follow the dosage instructions and check with your surgeon if you’re unsure.
When can I resume normal activities?
Light activities are usually fine after 24‑48 hours. Avoid heavy lifting, vigorous exercise, or swimming for at least a week, or until your doctor confirms it’s safe.
By knowing what to expect, recognizing the warning signs, and using proven self‑care tools, you can keep eye swelling under control and focus on the most important goal-restoring clear, comfortable vision.
 Sep, 1 2025
Sep, 1 2025

Selina M
September 1, 2025 AT 12:53thx for the guide love the easy steps!
Nicholai Battistino
September 7, 2025 AT 07:46Cold compresses are most effective within the first 48 hours.
Suraj 1120
September 13, 2025 AT 02:40Honestly the article downplays how quickly swelling can signal infection; many patients ignore subtle cues until it’s too late. The timeline you give feels overly optimistic for complex surgeries. You should stress that any persistent redness after 72 hours warrants a doctor’s visit. Also, the table oversimplifies steroid risks.
Shirley Slaughter
September 13, 2025 AT 02:41While I see your point, the guide does emphasize red‑flag symptoms clearly, and most surgeons follow strict post‑op protocols. It’s not about sugar‑coating; it’s about reassurance paired with vigilance. Remember, anxiety can worsen perceived swelling, so calm reassurance matters.
Sean Thomas
September 18, 2025 AT 21:33The real reason doctors push cold packs is to cut costs on more expensive anti‑inflammatory meds they’re paid to prescribe. Big pharma loves to keep patients on pricey eye drops, so they downplay simple home remedies. Keep an eye on what they’re not saying.
Aimee White
September 18, 2025 AT 21:35Oh, bravo! You’ve uncovered the grand ocular‑pharma conspiracy in 17 seconds flat. Next, we’ll be warned that water is a mind‑control fluid. Keep the drama alive, dear.
Javier Muniz
September 24, 2025 AT 16:26Great add‑on on staying hydrated – I’ve found drinking extra water actually reduces puffiness faster than any eye cream I’ve tried.
Sarah Fleming
September 24, 2025 AT 16:28Hydration is indeed the secret elixir, but let’s not forget the power of omega‑3s; they fight inflammation like a silent warrior.
Debra Johnson
September 30, 2025 AT 11:20It is imperative that patients adhere strictly to the prescribed post‑operative regimen; deviation may result in complications, including infection or delayed healing. Moreover, applying ice directly to the skin contravenes basic medical guidance and can cause frostbite – a preventable hazard. Therefore, I urge every reader to follow the instructions meticulously.
Andrew Wilson
September 30, 2025 AT 11:21yeah Debra nailed it – don’t skate on the ice thing, and stick to the schedule or you’ll be back for more appointments.
Kristin Violette
October 6, 2025 AT 06:13Post‑operative ocular edema is a multifactorial phenomenon driven by vascular permeability, inflammatory mediators, and mechanical disruption of tissue planes. From a physiological perspective, the breakdown of the blood‑aqueous barrier initiates a cascade of cytokine release, notably interleukin‑6 and prostaglandin E2, which orchestrate leukocyte infiltration. These cells, in turn, secrete matrix metalloproteinases that remodel extracellular matrix, facilitating fluid transudation into the subconjunctival space. Clinically, this manifests as the characteristic periorbital puffiness that peaks within the 12‑48 hour window as highlighted in the article. Quantitative studies using anterior segment optical coherence tomography have demonstrated a mean increase of 0.35 mm in conjunctival thickness during this phase. Importantly, patient‑specific factors such as pre‑existing dry eye, systemic hypertension, and variability in CYP450 enzyme activity modulate the intensity of the inflammatory response. Therapeutically, the judicious use of topical non‑steroidal anti‑inflammatory drugs (NSAIDs) provides cyclo‑oxygenase inhibition, thereby attenuating prostaglandin synthesis and reducing edema. Adjunctive cold therapy works via vasoconstriction, which can be quantified by a transient reduction in scleral blood flow measured by laser Doppler flowmetry. Elevating the head reduces hydrostatic pressure gradients, a principle well‑established in postoperative care of other organ systems, such as orthopedics. Nutritionally, omega‑3 fatty acids act as precursors to resolvins, specialized pro‑resolving mediators that actively switch off inflammation. From a pharmacokinetic standpoint, compliance with dosing intervals is critical; missed doses can prolong the half‑life of inflammatory mediators, delaying resolution. Moreover, while corticosteroid eye drops are potent, they carry the risk of iatrogenic ocular hypertension, necessitating periodic intra‑ocular pressure monitoring. Patients should also be cautioned against ocular rubbing, as mechanical trauma can re‑induce local cytokine release and compromise the healing epithelium. In summary, an interdisciplinary approach integrating pharmacology, ergonomics, and patient education yields the most efficient edema resolution. Adhering to these evidence‑based strategies not only accelerates visual recovery but also enhances overall patient satisfaction and outcomes.
Theo Asase
October 6, 2025 AT 06:15The drama of biochemical cascades is fascinating, but let’s not forget that the average person just wants their eyes back for a selfie without swelling.
Joey Yap
October 12, 2025 AT 01:06Contemplating the transient nature of swelling reminds us that even our bodies undergo cycles of excess and release, mirroring life's own ebbs and flows.
Lisa Franceschi
October 12, 2025 AT 01:08Indeed, the metaphorical parallel you draw is both apt and elegantly expressed; it underscores the importance of viewing postoperative care through both physiological and philosophical lenses.
Diane Larson
October 17, 2025 AT 20:00Always schedule your follow‑up – it’s the best safety net.