It starts small-a faint tingling in your toes, a weird numbness in your fingertips. You brush it off. Maybe it’s from standing too long. Or stress. Or sleeping funny. But if you’re taking certain medications, those quiet sensations could be your nerves sending out an early alarm. This isn’t just a minor annoyance. It’s medication-induced peripheral neuropathy, and catching it early can make all the difference.
What You’re Feeling: The Early Signs
Tingling and numbness from medications don’t feel like a pinprick or a limb that’s "fallen asleep." They’re persistent, often starting in your feet or hands and creeping upward like a glove or stocking being pulled on. You might notice it when you walk barefoot and your toes feel like they’re wrapped in cotton. Or when you button a shirt and your fingers just won’t respond the way they used to. These aren’t random glitches. They’re symptoms of nerve damage caused by drugs interfering with how your peripheral nerves send signals. The nerves in your hands and feet are the longest in your body, so they’re the first to show trouble. That’s why the pattern is so predictable: starts at the ends, moves inward. This is called a "stocking-glove" distribution. The good news? At this stage, it’s often mild. According to the National Cancer Institute’s grading system, this is Grade 1 neuropathy-symptoms are there, but they don’t interfere with daily life. You can still walk, type, and hold a cup. But if you ignore it, it can climb to Grade 2 or 3, where walking becomes painful, balance is off, and simple tasks get harder.Which Medications Cause This?
Not all drugs cause nerve damage. But some do-and often, they’re the ones you need most. Chemotherapy drugs are the biggest culprits. Oxaliplatin, used for colon cancer, causes tingling in up to 95% of patients during treatment. Paclitaxel, common in breast cancer, affects 60-70%. These aren’t side effects you can avoid-they’re built into how the drugs work. But knowing the risk lets you act fast. Antibiotics like isoniazid (for tuberculosis) and metronidazole (for infections) are also linked. About 10-20% of people on isoniazid develop symptoms, especially if they’re not taking vitamin B6 alongside it. Heart meds like amiodarone can cause neuropathy in 5-10% of long-term users. Even statins, the cholesterol-lowering pills millions take daily, are debated. Some studies suggest a tiny risk-around 1-2%-but others think the link is more about coincidence than causation. And then there are antiretrovirals for HIV, like stavudine, which can cause nerve damage in up to one-third of users. The key isn’t to stop taking your meds. It’s to recognize the signal before it turns into a scream.Why Early Detection Matters
A 2022 study in the Journal of Neuro-Oncology found that when cancer patients had their symptoms tracked monthly using simple checklists, the chance of their neuropathy worsening dropped by 37%. That’s huge. Because once nerves are severely damaged, recovery is slow-or sometimes impossible. Neurologists like Dr. Norman Latov from Weill Cornell Medicine say this plainly: "Early recognition is critical because many drug-induced neuropathies are reversible if the offending agent is discontinued promptly." But here’s the problem: most people don’t report these symptoms until they’re unbearable. A survey by the Foundation for Peripheral Neuropathy found that over half of patients waited three months or longer before telling their doctor. By then, the damage might already be done. Think of it like a smoke alarm. You don’t wait until the house is on fire to check the battery. The tingling? That’s the beep.
What Doctors Look For
Your doctor doesn’t need an MRI to spot early neuropathy. They’ll ask you to describe the sensations, check your reflexes, test your sensitivity to light touch or vibration, and maybe use a tuning fork on your big toe. Some clinics now use tools like the Total Neuropathy Score or the EORTC QLQ-CIPN20 questionnaire-standardized forms that track changes over time. These aren’t just paperwork. They help spot trends before you even notice them. In advanced cases, nerve conduction studies may be used. But at the mild stage, those often come back normal. That’s why patient-reported symptoms matter more than tests at first. New tools are emerging, too. The FDA-approved SudoScan device measures sweat response through the skin-a sign of small nerve fiber damage. It’s not in every doctor’s office yet, but it’s becoming more common in cancer centers.What You Can Do Right Now
If you’re on a high-risk medication and notice tingling or numbness:- Don’t ignore it. Write down when it started, where it is, and how bad it feels on a scale of 1 to 10.
- Tell your doctor immediately. Don’t wait for your next appointment. Call the nurse line or send a message through your portal.
- Ask about dose adjustments. You might not need to stop the drug. Studies show 60-70% of patients can keep taking their treatment with a reduced dose or longer breaks between cycles.
- Check for supplements. If you’re on isoniazid, ask about vitamin B6 (pyridoxine). It’s often prescribed alongside it to lower risk.
- Protect your feet. Check them daily for cuts or blisters. Wear shoes indoors. Use non-slip mats in the bathroom. Numb feet don’t feel pain-and that’s how ulcers and infections start.
Real Stories, Real Consequences
One user on CancerCare shared: "My first sign was just tingling in my toes after my second oxaliplatin treatment. My oncologist said it was normal. By cycle 4, I couldn’t button my shirts." She eventually had to stop treatment early. Another on Reddit said: "Started noticing numbness in fingers after 3 months of isoniazid. My doctor increased my B6 but didn’t stop the meds. Now 6 months later, still have tingling despite stopping." But there are wins, too. On PatientsLikeMe, 73% of people who stopped the drug at the first sign of tingling saw their symptoms disappear or nearly vanish within six months. The difference? Timing.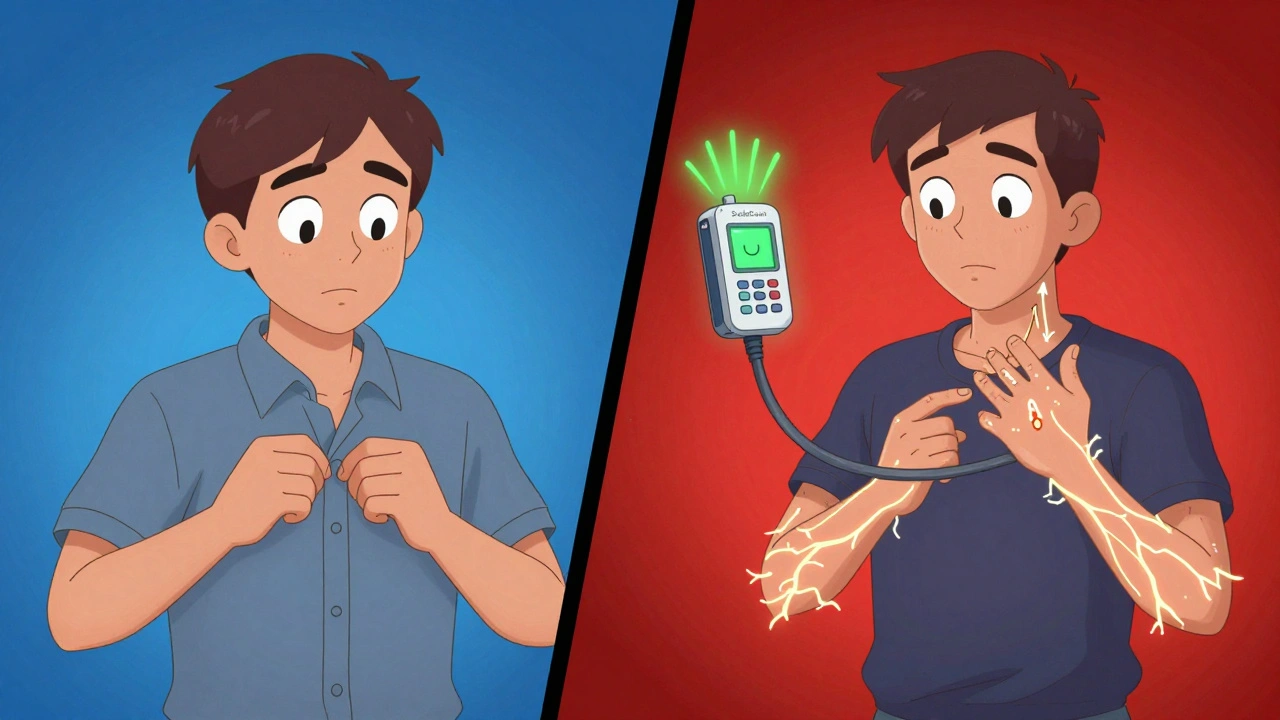
What’s Changing in 2025
The field is shifting. In 2023, the Peripheral Nerve Society updated its guidelines to include quantitative sensory testing-a way to detect nerve changes before symptoms even appear. That means in the near future, you might get a simple, painless test before starting chemotherapy to see if you’re genetically more at risk. Dr. Charles Loprinzi from Mayo Clinic predicts: "Within five years, genomic risk stratification will become standard before initiating neurotoxic chemotherapy." Clinical trials are also testing protective agents like acetyl-L-carnitine. Early results show a 40% reduction in symptom severity for patients on paclitaxel. The goal isn’t to avoid life-saving drugs. It’s to use them smarter.When to Worry
Mild tingling? Likely manageable. But if you start experiencing:- Weakness in your hands or feet
- Difficulty walking or balancing
- Sharp, burning pain that keeps you up at night
- Loss of coordination or frequent tripping
Bottom Line
Tingling and numbness from medications aren’t something to tolerate. They’re a warning sign-and one you can act on. Whether you’re on chemo, antibiotics, or heart meds, knowing the risks and speaking up early gives you control. You don’t have to choose between healing your body and protecting your nerves. With the right info and timing, you can do both.Can medication-induced tingling go away on its own?
Yes, in many cases-especially if caught early. About 70% of patients who stop or adjust the medication at the first sign of mild tingling or numbness see improvement within 3 to 6 months. But if the drug continues and nerve damage worsens, recovery becomes slower and less complete. The earlier you act, the better your chances.
Is vitamin B6 helpful for neuropathy from medications?
It’s proven helpful for neuropathy caused by isoniazid (used for tuberculosis). Taking 50 mg of vitamin B6 daily while on isoniazid reduces the risk of nerve damage by up to 70%. For other drugs like chemotherapy, evidence is weaker. Always ask your doctor before starting any supplement-it can interfere with some treatments.
Do statins cause tingling and numbness?
The link is controversial. Some patients report symptoms, but large studies haven’t confirmed a strong causal relationship. Experts like Dr. Christopher H. Gibbons from Harvard suggest the connection may be due to reporting bias-people notice symptoms after hearing about the risk. If you’re concerned, talk to your doctor about alternatives, but don’t stop statins without medical advice-they’re critical for heart health.
How long does it take for symptoms to appear after starting a drug?
It varies. For chemotherapy drugs like oxaliplatin, tingling can start after just one or two doses. For antibiotics like metronidazole or isoniazid, it often takes 1 to 3 months. Statins and heart meds may take even longer-sometimes over a year. The key is monitoring from the start, not waiting for symptoms to become severe.
Should I stop my medication if I feel tingling?
Never stop a prescribed medication on your own. Instead, contact your doctor right away. In many cases, the dose can be lowered, the schedule adjusted, or a protective supplement added. Stopping abruptly can be dangerous-especially with cancer drugs or heart medications. Your doctor can help you balance treatment benefits against nerve risks.
Are there tests to confirm medication-induced neuropathy?
Yes, but they’re not always needed at first. Doctors usually start with a physical exam and symptom history. If it’s unclear, they may order nerve conduction studies or use tools like SudoScan, which measures skin conductance to detect early small-fiber damage. In research settings, quantitative sensory testing can spot changes before you feel them. But diagnosis is often based on timing: symptoms started after beginning the drug and improved after stopping it.
Can I prevent medication-induced neuropathy?
You can’t always prevent it, but you can reduce your risk. Stay alert to early symptoms. Ask your doctor about protective strategies-like vitamin B6 for isoniazid or dose scheduling for chemo. Avoid alcohol, which can worsen nerve damage. Keep your blood sugar under control if you’re diabetic. And don’t skip follow-up appointments. Monitoring is your best defense.
 Dec, 3 2025
Dec, 3 2025

Elizabeth Crutchfield
December 4, 2025 AT 13:33i kept ignoring the tingling in my toes till i couldn't button my jeans... then i realized it wasn't just "sleeping wrong". thanks for saying this out loud.
Ben Choy
December 5, 2025 AT 06:50this hit me right in the feels 😔
my dad was on isoniazid for TB and never told anyone about the numbness till his feet felt like bricks. he's okay now, but only because he finally spoke up. please, if you feel it-say something. it's not "just a side effect".
Emmanuel Peter
December 7, 2025 AT 05:12lol so now we're blaming statins for everything? i've got 40k people on statins and 3 of them reported tingling. that's not causation, that's confirmation bias. you people read one reddit thread and think you're neurologists now. get a nerve conduction study before you panic.
Heidi Thomas
December 7, 2025 AT 16:11you're all overreacting. if you're on chemo you're gonna have side effects. stop being dramatic. the real problem is people who don't understand that medicine isn't magic. if you want zero side effects go drink herbal tea and pray.
Alex Piddington
December 8, 2025 AT 08:29Thank you for this thoughtful and well-researched post. I've seen too many patients delay reporting symptoms out of fear or misinformation. Early intervention truly changes outcomes. Please continue sharing these vital details. 🙏
Libby Rees
December 9, 2025 AT 16:14My aunt had this with metronidazole. She didn't tell her doctor for six months. By then, she couldn't walk without a cane. She's better now, but it took a year. Don't wait. Write it down. Tell someone.
Rudy Van den Boogaert
December 10, 2025 AT 06:36My oncologist had me use this checklist every week during chemo. It was just five questions: tingling? numbness? cold sensitivity? balance off? weak grip? I tracked it on my phone. When it went from 1/10 to 4/10, we lowered my dose. I finished treatment. Still have a little tingle, but I can feel my toes again. This stuff works.
I know it sounds boring, but writing it down is the difference between "oh it's fine" and "oh crap, we need to act."
My nurse said most people don't even notice the numbers are climbing until they're at 8/10. Don't be that person.
Also, wear socks to bed if your feet get cold. Cold makes the tingling worse. Just a little thing, but it helps.
And yes, vitamin B6 helps with isoniazid. I took it with mine. Didn't get any numbness. My doc said it's like a seatbelt for your nerves.
Don't be shy about asking. Your doctor wants you to speak up. They're not mad you noticed something. They're glad you did.
Martyn Stuart
December 12, 2025 AT 01:35For anyone on oxaliplatin: the tingling gets worse with cold-cold drinks, cold air, even touching a metal doorknob. I learned this the hard way. Now I wear gloves to open the fridge, use warm water to wash dishes, and never hold ice cubes. It’s not a cure, but it reduces flare-ups. Also-ask about cryotherapy gloves/socks. They’re weird, but they work. My oncology center gives them out now.
And yes, the 73% recovery rate on PatientsLikeMe? Real. My cousin stopped chemo at grade 1. Within 4 months, her fingers felt normal again. She’s back to knitting. Don’t wait for it to get bad.
And if your doctor says "it’s normal," ask: "What’s the protocol for grade 1?" If they don’t have one, ask for a referral. You deserve better.