Medication-Induced Hyponatremia Risk Checker
This tool helps you assess your risk of developing severe hyponatremia (low sodium) from medications. Based on your medication use, age, gender, and symptoms, you'll receive an immediate risk assessment. Hyponatremia can develop quickly—especially with certain drugs—and requires prompt attention.
Medication Risk Assessment
Your Risk Assessment
Enter your information to see your risk level.
Low sodium isn’t just a lab number-it can turn a calm morning into a medical emergency. When certain medications disrupt your body’s sodium balance, confusion, seizures, and even coma can follow in just days. This isn’t rare. In fact, hyponatremia from drugs is one of the most common and dangerous electrolyte problems seen in hospitals today, especially in older adults and people taking antidepressants or seizure medications.
What Exactly Is Hyponatremia?
Hyponatremia means your blood sodium level has dropped below 135 mmol/L. Severe cases-when it falls under 120 mmol/L-can be life-threatening. Sodium isn’t just about salt on your food. It’s critical for nerve and muscle function, fluid balance, and brain health. When sodium dips too low, water floods into your brain cells, causing them to swell. That’s when symptoms start.
Unlike slow-developing conditions, medication-induced hyponatremia often hits fast. People start feeling off-headaches, nausea, fatigue-and within a week or two, they might be confused, stumbling, or having seizures. The brain doesn’t adapt quickly enough when the drop is sudden, and that’s what makes drug-related cases so dangerous.
Which Medications Cause the Most Problems?
Not all drugs cause this-but some carry a much higher risk. The top offenders are:
- Diuretics (like hydrochlorothiazide): Responsible for nearly 3 in 10 cases. They make you pee out more water than salt, diluting sodium.
- SSRIs (sertraline, citalopram, fluoxetine): These antidepressants trigger SIADH-a condition where your body holds onto too much water. About 22% of medication-induced hyponatremia cases come from these drugs.
- Antiepileptics (carbamazepine, oxcarbazepine): Carbamazepine has over five times the risk compared to non-users. Many patients don’t know this until it’s too late.
- MAOIs, ACE inhibitors, NSAIDs, and MDMA: Less common, but still documented causes.
Here’s the scary part: These drugs are prescribed to millions. In the UK and US, SSRI use has climbed nearly 20% since 2018. That’s why hyponatremia cases are rising too-4.2% each year. And most people never get warned.
The Warning Signs You Can’t Ignore
Early symptoms are easy to brush off. You might think it’s the flu, stress, or just getting older. But if you’re on one of these drugs and notice:
- Unexplained nausea or vomiting
- Headaches that won’t go away
- Feeling unusually tired or weak
- Confusion or trouble concentrating
- Muscle cramps or spasms
-it’s time to get checked. In severe cases (sodium below 115 mmol/L), seizures happen in about 1 in 5 patients. Around 37% of people with sodium this low die if untreated for more than 48 hours. And confusion can turn to coma in as little as 6-8 hours.
One nurse on Reddit shared a case where a 72-year-old patient developed a grand mal seizure just 10 days after starting sertraline. The doctor had dismissed the early nausea and headache as “normal side effects.” That’s not normal. That’s a red flag.
Why Are Older Adults and Women at Higher Risk?
Over 60% of severe medication-induced hyponatremia cases happen in people over 65. Why? Aging kidneys don’t regulate water as well. Older adults also take more medications, often in combination. And women are affected more frequently-57% of cases are female. Hormonal differences and lower body weight may play a role.
It’s not just age or gender. It’s also how long you’ve been on the drug. Most severe cases show up within the first 30 days. That’s why routine sodium checks during this window are critical. Yet, only 63% of doctors follow recommended monitoring guidelines.
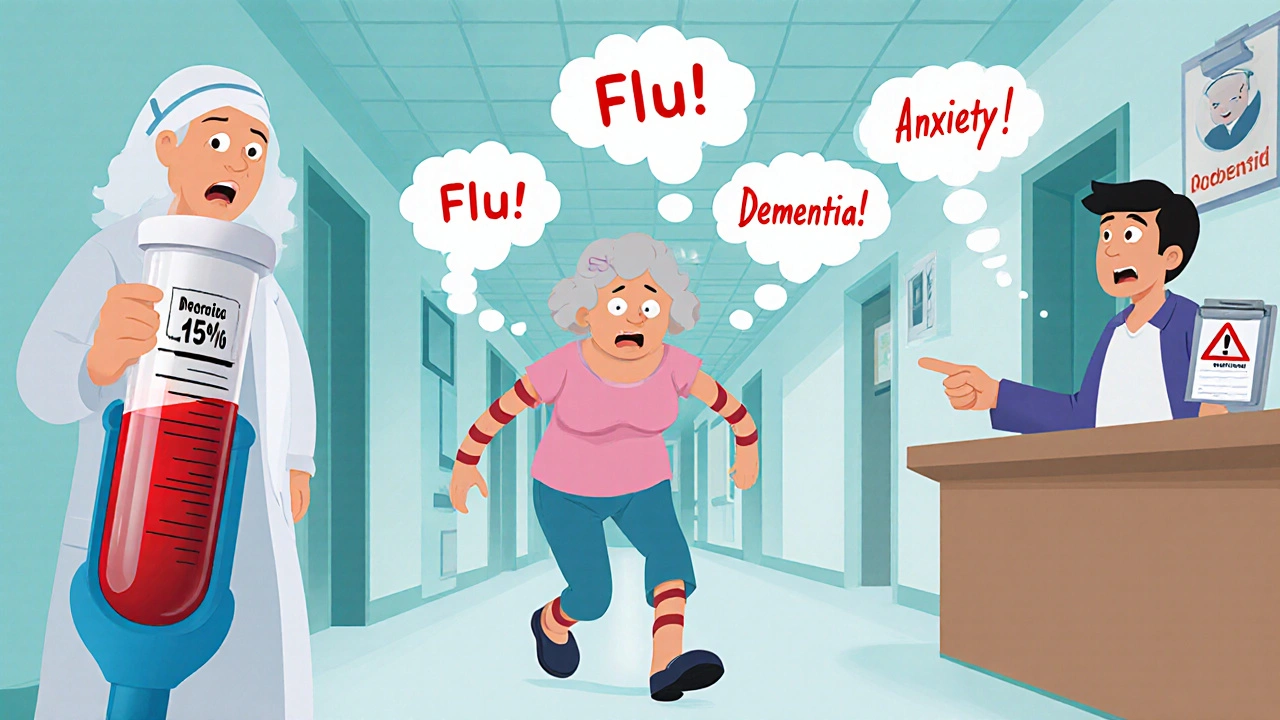
How Is It Diagnosed-and Misdiagnosed?
Doctors often miss this. In emergency rooms, 31% of hyponatremia cases are initially misdiagnosed. Common mistakes:
- Calling it “the flu” (29% of cases)
- Labeling it as anxiety or depression (21%)
- Assuming it’s early dementia (18%)
On patient forums, 68% report being misdiagnosed before getting the right blood test. One patient wrote: “I was told I was having panic attacks-turns out my sodium was 118. I spent five days in the hospital.”
The fix? A simple blood test. If you’re on a high-risk medication and have new neurological symptoms, ask for a serum sodium level. No need to wait. The Hyponatremia Algorithm from the European Hyponatremia Network helps doctors spot drug causes with 89% accuracy if used early.
How Is It Treated?
Correction must be careful. Too fast, and you risk osmotic demyelination syndrome-a rare but devastating brain injury. The goal is to raise sodium by no more than 6-8 mmol/L in the first 24 hours.
Treatment depends on severity:
- Mild cases: Stop the drug, limit fluids, monitor.
- Severe cases (with seizures or coma): IV saline, sometimes with drugs like tolvaptan (Samsca), approved in late 2023 for this exact use.
Recovery is good-if caught early. 92% of patients recover fully if treated within 24 hours. That drops to 67% if treatment is delayed beyond 48 hours. Time isn’t just important-it’s everything.
Can It Happen Again?
Yes. If you need to stay on the drug-for example, if you’re on an SSRI for depression-recurrence rates are high. About 33% of people on long-term SSRIs develop hyponatremia again. That’s why ongoing monitoring is non-negotiable. For diuretics, switching to another type can cut recurrence to 12%.
Some patients are lucky enough to catch it early. One Mayo Clinic patient shared: “My pharmacist caught the interaction between oxcarbazepine and my other meds before I even filled the prescription. Saved me from what happened to my sister.”

What Can You Do to Protect Yourself?
You don’t have to wait for a seizure to get answers. Here’s what works:
- Ask your doctor if your medication carries a risk of low sodium. Don’t assume they’ll bring it up.
- Request a blood test within 7 days of starting a new high-risk drug-and again at 2 and 4 weeks.
- Know the symptoms. If you feel confused, nauseous, or unusually tired after starting a new pill, don’t wait.
- Talk to your pharmacist. They see drug interactions daily. Many now flag hyponatremia risk at the counter.
- Track your symptoms. Keep a simple log: “Day 3: Headache, nausea.” That helps your doctor connect the dots.
AI tools are starting to help too. Mayo Clinic’s pilot system predicts hyponatremia risk 72 hours before symptoms appear-by analyzing your EHR data. It’s not everywhere yet, but it’s coming.
What’s Changing in 2025?
The FDA now requires stronger warnings on 27 high-risk medications. The European Medicines Agency now mandates that pharmacists educate patients on sodium risks at the time of prescription.
But the biggest shift? Awareness. More hospitals are screening older patients on SSRIs or antiepileptics routinely. Community clinics lag behind-only 47% do it, compared to 82% in academic centers. That gap kills people.
By 2028, cases are expected to rise 22% due to aging populations. But with better screening, severe complications could drop by up to 38%.
Final Thought: Don’t Wait for a Seizure
Hyponatremia from medications isn’t a mystery. It’s predictable. Preventable. And far too often, ignored. The window between feeling off and having a seizure is sometimes less than half a day. If you’re on an SSRI, diuretic, or seizure drug-and you’re over 65, or a woman-ask for a sodium test. Don’t wait for someone else to notice something’s wrong. You’re the first line of defense.
Can antidepressants really cause seizures from low sodium?
Yes. SSRIs like sertraline and citalopram can trigger SIADH, a condition where the body retains too much water, diluting sodium. When sodium drops below 115 mmol/L, seizures can occur. About 22% of all medication-induced hyponatremia cases come from SSRIs. Symptoms often start within 1-4 weeks of starting the drug.
How long does it take for hyponatremia to develop after starting a new medication?
Most cases appear within the first 30 days. The fastest drops happen in the first 7-10 days. For example, one patient’s sodium fell 0.8 mmol/L per day after starting sertraline-leading to seizures by day 10. That’s why checking sodium levels at 7 days is a key safety step.
Is hyponatremia from drugs more dangerous than other causes?
It’s not necessarily more dangerous-but it’s more sudden. Unlike hyponatremia from kidney disease or heart failure, which develops slowly, drug-induced cases often drop rapidly. The brain doesn’t have time to adapt, so neurological symptoms like confusion and seizures appear faster. But if caught early, recovery rates are better-92% if treated within 24 hours.
Can I just stop the medication if I think I have low sodium?
No. Stopping abruptly can be dangerous, especially with antidepressants or seizure meds. You need medical supervision. Stopping too fast can cause withdrawal or rebound seizures. Always consult your doctor. They may adjust your dose, switch medications, or give you IV fluids to correct sodium safely.
Are there any new treatments for drug-induced hyponatremia?
Yes. Tolvaptan (Samsca), approved in November 2023, is now an option. It helps your body get rid of excess water without losing sodium. In trials, it cut time to correction by 34% compared to standard care. It’s especially useful for people who need to keep taking their medication but can’t tolerate low sodium.
Should I get my sodium checked if I’m on a diuretic?
Absolutely. Diuretics cause nearly 30% of all medication-induced hyponatremia cases. The American Geriatrics Society recommends checking sodium within 7 days of starting a diuretic-and again at 2 and 4 weeks, especially if you’re over 65. Even if you feel fine, a simple blood test can catch a dangerous drop before symptoms start.
 Nov, 1 2025
Nov, 1 2025

Patrick Merk
November 16, 2025 AT 01:52Man, I had no idea SSRIs could do this. My aunt was on sertraline for years and kept saying she felt "off"-like her brain was underwater. We thought it was just aging. Turns out her sodium was at 119. She spent a week in the hospital. Never even crossed our minds to ask for a blood test. Thanks for spelling this out so clearly.
Koltin Hammer
November 16, 2025 AT 22:40Look, I get it-meds save lives. But we’re treating depression like it’s a broken pipe you just slap a new valve on and walk away. This isn’t just about sodium levels, it’s about how we’ve outsourced our health to pills and assumed the system has our back. Turns out, the system’s busy filling out forms while your brain cells are swelling like balloons. I’m not saying ditch the meds-I’m saying demand better monitoring. Ask for the test. Don’t wait until you’re seizing in the grocery store.
Phil Best
November 17, 2025 AT 16:27So let me get this straight. We’ve got millions of people popping antidepressants like M&Ms, and the only warning label is "may cause mild nausea"? Meanwhile, your brain is slowly turning into a water balloon. And the doctor says, "It’s just side effects, honey." Oh, I’m sorry-did I forget to mention I’m 70 and my kidneys have been on vacation since 2012? This isn’t medicine, it’s Russian roulette with a prescription pad.
Parv Trivedi
November 18, 2025 AT 23:22Thank you for sharing this important information. In my country, many elderly patients are prescribed multiple medications without proper monitoring. This article is a wake-up call. I will share it with my family and community. Simple blood tests can prevent tragedy. Awareness saves lives.
Willie Randle
November 20, 2025 AT 20:11Let’s be precise: hyponatremia is not "caused" by medications-it’s a consequence of pharmacologically induced SIADH or renal water retention. The distinction matters because blaming the drug ignores the physiological cascade. Also, the 92% recovery rate applies only to cases corrected within 24 hours with controlled correction rates. Overcorrection leads to ODS, which is often permanent. So yes-get tested. But also understand what you’re testing for.
Connor Moizer
November 20, 2025 AT 20:50Why are we still talking about this like it’s news? This has been documented since the 90s. Your doctor doesn’t care. Your pharmacist doesn’t care. The FDA only updated warnings because someone died on national TV. You want to stay alive? Stop trusting people who have 3 minutes to talk to you. Test your sodium. Track your symptoms. If you’re on a diuretic or SSRI and you’re over 50, you’re playing with fire-and you’re the only one holding the lighter.
kanishetti anusha
November 21, 2025 AT 01:00I’m a nurse in rural India, and we see this all the time. Elderly patients on hydrochlorothiazide for hypertension, no labs done for months. They get confused, we think dementia, then we find sodium at 114. It’s heartbreaking. I wish we had the resources to test everyone-but even just asking, "Have you felt dizzy or nauseous since starting this pill?" can save someone. Thank you for highlighting this.
roy bradfield
November 21, 2025 AT 01:09They don’t want you to know this. The pharmaceutical giants? They profit from chronic conditions. If you fix hyponatremia early, you reduce hospitalizations. Less hospitalizations = less profit. That’s why they bury the warnings in 12-point font. And why doctors ignore it-because they’re paid per visit, not per outcome. They don’t want you to ask for a blood test. They want you to keep coming back. This isn’t negligence-it’s business. And you’re the product.
Liam Dunne
November 23, 2025 AT 00:13My dad was on carbamazepine for seizures. Got confused, started stumbling. Doctor said "old age." We pushed for a panel. Sodium was 116. He was in ICU for 3 days. They switched him to lamotrigine. No more issues. Point is: if you’re on one of these drugs and feel weird-don’t wait. Push. Hard. You’re not being difficult. You’re being smart.
Vera Wayne
November 23, 2025 AT 09:31Thank you, thank you, THANK YOU for this. I’m a 68-year-old woman on sertraline for anxiety, and I’ve had headaches for three weeks. I thought it was stress. I just requested my sodium levels today. I feel like I’ve been given a second chance. Please, everyone-don’t wait. Ask. Now.
Rodney Keats
November 24, 2025 AT 08:08Wow. So the real takeaway is: if you’re on meds and you’re not dead yet, you’re just being slowly liquefied by Big Pharma’s fine print. Congrats, you’re the main character in a horror movie where the villain is your pharmacist.