By the time you hit 50, your bones are already losing ground. Not because you’re getting old, but because you probably didn’t give them the right support when it mattered most. Osteoporosis isn’t just a ‘women’s issue’ or something that happens to elderly people. It’s a silent thief - stealing strength from your skeleton without warning, until you trip, cough too hard, or bend over and hear a snap. And then it’s too late.
What Actually Happens When Bone Density Drops?
Your bones aren’t static. They’re alive, constantly being broken down and rebuilt. Up until your late 20s, your body builds more bone than it loses. That’s your peak bone mass. After that, the balance shifts. For most people, bone loss starts at about 0.3% to 0.5% per year. But for women after menopause, that rate jumps to 2% to 3% - for five to seven years straight. That’s like losing a full year’s worth of bone in just six months. This isn’t just about aging. It’s about imbalance. When your body breaks down bone faster than it can rebuild it, your internal structure becomes porous, like a sponge with holes. The trabeculae - the tiny internal struts that give bone its strength - thin out and disconnect. What used to be a sturdy lattice turns into a fragile grid. That’s when a fall from standing height, or even a sneeze, can cause a fracture.Who’s Most at Risk? The Real Numbers
You might think osteoporosis only affects older women. But the data tells a more detailed story.- One in three women over 50 will suffer an osteoporotic fracture. For men? One in five.
- White and Asian women have a 1.7 times higher risk than Black women.
- If your parent broke a hip, your risk goes up by 60% to 80%.
- Women who hit menopause before 45 have more than double the risk compared to those who go through it naturally in their 50s.
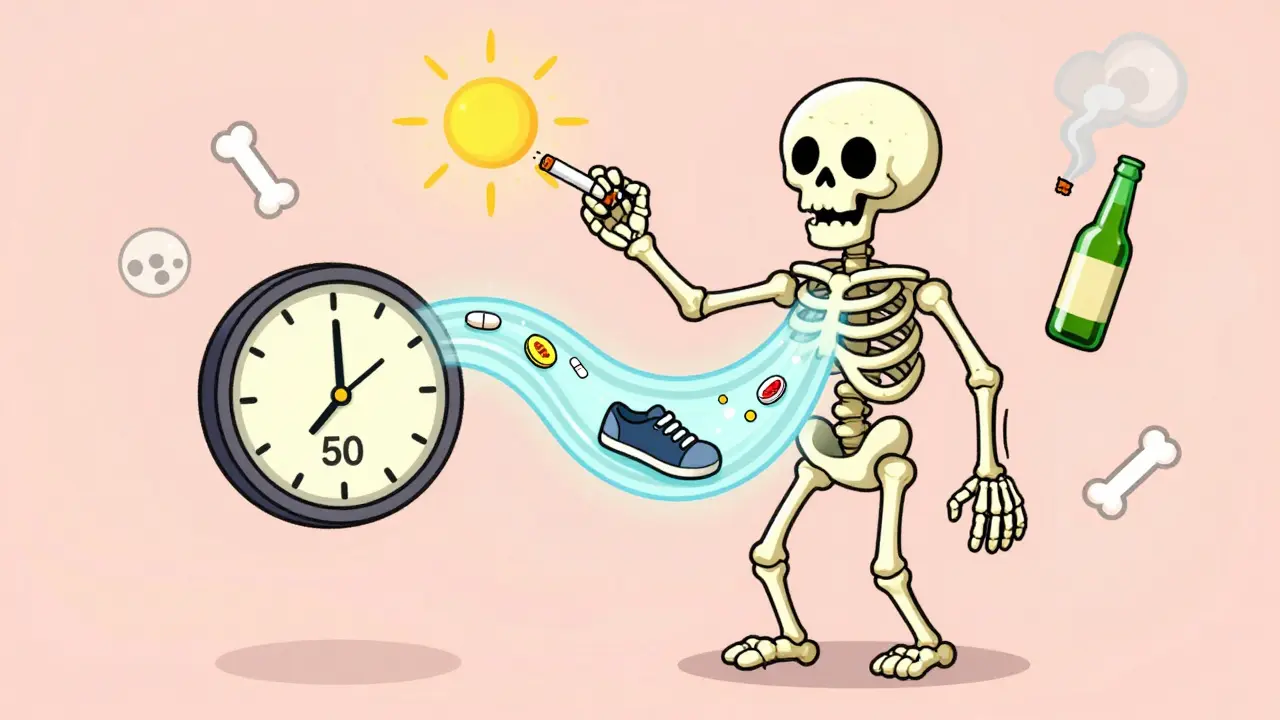
The Big 5 Modifiable Risks (And How to Fix Them)
You can’t change your age or your genes. But you can control these five things - and each one has a direct, measurable impact on your bone health.1. Calcium: The Missing Piece
Most adults need 1,000 mg of calcium a day. Seniors need 1,200 mg. But here’s the problem: you can’t just take a big pill and call it done. Your body absorbs calcium best in small doses - 500 to 600 mg at a time, with meals.- One cup of fortified milk = 300 mg
- One cup of cooked kale = 180 mg
- Three ounces of canned sardines with bones = 325 mg
2. Vitamin D: The Hidden Driver
You need vitamin D to absorb calcium. No vitamin D? Your calcium just passes through. And here’s the scary part: 42% of U.S. adults have levels below 20 ng/mL - the threshold for deficiency. Aim for 800-1,000 IU per day. If you’re deficient, you may need 2,000 IU daily for 3-4 months to catch up. Sunlight helps, but in the UK, you can’t rely on it from October to March. That’s why supplementation isn’t optional - it’s essential.3. Smoking: The Bone Killer
Smoking doesn’t just hurt your lungs. It cripples your bones. Nicotine cuts blood flow to bone tissue, slows down bone-building cells, and interferes with estrogen. One pack a day increases your fracture risk by 55%. Quitting doesn’t reverse all the damage - but it stops the bleeding. Within a year of quitting, your bone loss slows to normal rates.4. Alcohol: The Silent Saboteur
More than two drinks a day? You’re increasing your hip fracture risk by 41%. Alcohol messes with calcium balance, lowers testosterone in men, and increases your chance of falling. It’s not about occasional wine with dinner. It’s about daily habits. One drink is fine. Two or more? That’s a red flag.5. Inactivity: The Slow Motion Collapse
Bones need stress to stay strong. No load? No growth. Sitting all day is like letting your bones rust. Weight-bearing exercise - walking, climbing stairs, dancing, hiking - tells your body: “Keep building.” Resistance training - lifting weights, using resistance bands - adds even more protection. The goal? 30 to 45 minutes of weight-bearing activity five days a week, plus two days of strength training. Studies show this cuts fracture risk by 30-40%. And you don’t need to run marathons. Brisk walking 20 minutes a day, five times a week, makes a difference.
Fracture History: The Strongest Predictor of the Next One
Here’s the most important thing no one tells you: if you’ve already had one fragility fracture, your chance of another one skyrockets.- After a vertebral fracture, your risk of another spinal fracture jumps by 86%.
- After a hip fracture, your risk of another hip fracture goes up by 200%.
Medications: When to Consider Them
Not everyone needs drugs. But if your FRAX score shows a 20% or higher chance of a major fracture in 10 years, medication can be life-changing.- Bisphosphonates (like alendronate or risedronate) are first-line. They slow bone loss. But up to 58% of people stop them because of stomach upset or jaw pain.
- Romosozumab (Evenity), approved in 2023, actually builds new bone while slowing breakdown. It’s for high-risk patients and works fast - 73% fewer spine fractures in a year.
- Denosumab is an injection every six months. It’s strong, but if you stop it, bone loss can rebound quickly.

Preventing Falls: The Final Line of Defense
Even the weakest bone won’t break if you don’t fall. That’s why fall prevention is just as important as bone building.- Remove rugs and clutter from floors.
- Install grab bars in the bathroom.
- Use non-slip mats in the shower.
- Get your vision checked yearly.
- Review your medications - some cause dizziness.
- Do balance exercises: stand on one foot while brushing your teeth, walk heel-to-toe, try tai chi.
The Real Bottom Line
Osteoporosis isn’t inevitable. It’s preventable - but only if you act before it’s too late. The best time to build strong bones was 20 years ago. The second best time is now. Start today:- Get your vitamin D levels checked - if you’re over 50, assume you’re low.
- Drink milk, eat leafy greens, or take a calcium supplement with meals.
- Walk 30 minutes five days a week. Lift something heavy twice a week.
- Quit smoking. Cut back on alcohol.
- If you’ve had a fracture after 50, demand a bone density test.
- Make your home safer - before you need to.
Can you reverse osteoporosis naturally?
You can’t fully reverse advanced osteoporosis, but you can stop it from getting worse - and even rebuild some bone. Weight-bearing exercise, adequate calcium and vitamin D, quitting smoking, and avoiding excessive alcohol can improve bone density by 1% to 3% per year. In some cases, medications like romosozumab can increase bone mass by 7% to 10% in a year. But without intervention, bone loss continues. The goal isn’t to return to 25-year-old bone density - it’s to prevent fractures and stay strong.
Do I need a bone density test if I’m not a woman?
Yes. While women are at higher risk, one in five men over 50 will have an osteoporotic fracture. Men should get tested if they’re over 70, or if they’re over 50 and have risk factors: low body weight, smoking, long-term steroid use, a prior fracture, or a condition like rheumatoid arthritis or type 1 diabetes. Don’t assume it’s only a women’s issue.
Is dairy the only good source of calcium?
No. While milk and yogurt are easy sources, you can get calcium from canned salmon with bones, sardines, fortified plant milks (soy, almond, oat), tofu made with calcium sulfate, kale, bok choy, broccoli, and almonds. One cup of cooked collard greens has more calcium than a cup of milk. The key is variety and consistency - not just dairy.
Can osteoporosis cause pain?
Osteoporosis itself doesn’t hurt. But when it leads to fractures - especially spinal ones - pain follows. A collapsed vertebra can cause sudden, severe back pain, loss of height, or a curved spine. Many people think it’s just “aging back pain,” but it’s often a silent fracture. If you’re over 50 and have new back pain without injury, get it checked.
How long does it take to see results from bone-strengthening efforts?
Bone changes slowly. You won’t see results on a scan until after 6 to 12 months of consistent exercise, calcium, and vitamin D. But you’ll feel better sooner - better balance, more strength, less fear of falling. Those are early wins. The scan is just confirmation. Stick with it. Bone health is a marathon, not a sprint.
Are there foods that hurt bone health?
Yes. Excess salt pulls calcium out of your bones. Too much caffeine (more than 3 cups of coffee a day) can interfere with absorption. Colas may have phosphoric acid that disrupts calcium balance, though the evidence is mixed. The biggest issue isn’t one food - it’s the overall diet. A diet low in protein, fruits, and vegetables increases fracture risk. Focus on whole foods, not just avoiding the bad ones.
 Jan, 7 2026
Jan, 7 2026
Prakash Sharma
January 8, 2026 AT 14:18Finally someone speaks truth! In India, we think osteoporosis is a Western disease-until your grandma breaks her hip falling off the charpai. We ignore calcium because 'ghee and roti are enough.' Bullshit. My uncle died from a spine fracture at 62. No one tested him. No one cared. Start early. Eat dals, paneer, leafy greens. Stop pretending age is destiny.
Donny Airlangga
January 10, 2026 AT 05:44This hit me hard. My mom had a vertebral fracture last year and didn’t even realize it until her posture changed. She thought it was just ‘getting old.’ I didn’t know how much damage alcohol and sitting all day were doing. I’m getting her tested this week. Thank you for making this so clear.
Evan Smith
January 11, 2026 AT 14:03So let me get this straight… I can’t just chug milk and call it a day? I thought I was doing great because I drink one glass a week. 😅 Also, why is everyone suddenly talking about sardines? Are we all going to start eating fish bones like pirates now?
Manish Kumar
January 11, 2026 AT 22:41Think about it-our bones are not just scaffolding, they’re living archives of our choices. Every cigarette, every soda, every hour spent staring at a screen-it’s etched into the trabeculae. We live in a culture that worships youth but neglects the very structure that holds us upright. The body doesn’t lie. It whispers until it screams. And when it screams, it’s already too late. You can’t buy back time. But you can choose to walk differently today. Not for the scan. Not for the doctor. For the day you bend down to tie your shoe and don’t wince.
christy lianto
January 12, 2026 AT 00:20STOP waiting until you’re 60. I started walking 20 minutes a day at 45. Took supplements. Cut out soda. Two years later, my DXA scan showed a 2% increase. Not because I’m special-because I showed up. You don’t need to run marathons. Just move. Every damn day. Your future self will thank you.
Annette Robinson
January 13, 2026 AT 21:09So many people think bone health is just for women or the elderly. But men-especially those with sedentary jobs or who smoke-are silently losing bone density. If you’re over 50 and haven’t been tested, please, talk to your doctor. It’s not scary. It’s empowering. You’re not broken-you’re just overdue for a check-in.
Dave Old-Wolf
January 15, 2026 AT 04:07Wait-so if I quit smoking, my bone loss slows to normal? That’s it? No magic? No miracle cure? Just… stop smoking? Huh. Guess I’ve been overcomplicating this whole thing.
Molly Silvernale
January 15, 2026 AT 07:44Bones… are poems written in calcium and collagen… each step, a stanza… each lift, a rhyme… and when we forget to move… the verses crumble… silently… like autumn leaves… no one notices… until the wind blows… and the whole tree collapses…
Ken Porter
January 15, 2026 AT 21:56Just read the CDC’s STEADI guidelines. Same advice. 29% reduction. No magic. No pills. Just clean floors and balance exercises. Why do people need a 3000-word essay to realize they should stop tripping over their own rugs?
swati Thounaojam
January 16, 2026 AT 16:58my mom used to eat kale but never took vit d… now she’s on meds… i wish she knew sooner…
Luke Crump
January 17, 2026 AT 08:26Oh great. Another ‘you’re dying if you don’t drink milk and lift weights’ scare piece. What about the Okinawans? They live to 100 eating rice and tofu with no calcium supplements. Maybe the problem isn’t your bones-it’s the medical-industrial complex selling you fear and pills.
Aubrey Mallory
January 17, 2026 AT 10:32For everyone who thinks this doesn’t apply to them: I’m a 58-year-old man who broke my wrist lifting a suitcase. No fall. No trauma. Just… bone gave way. I didn’t know I was at risk. Now I do. And I’m doing the work. You can too. It’s not about being perfect. It’s about being consistent. Start small. Stay steady.
Kristina Felixita
January 17, 2026 AT 22:57As someone raised in a family that never talked about health… this is the first time I’ve felt like someone actually saw me… my grandma had 3 fractures… no one knew why… we just said ‘she was frail’… but it wasn’t frailty… it was neglect… i’m starting with walking… and i’m gonna make my kids do it too… even if they roll their eyes…