Oral Thrush Prevention Calculator
Prevention Calculator
Oral thrush risk is significantly reduced with proper rinsing after medication use. Calculate your personalized risk reduction below.
Prevention Results
0%
Risk Reduction
Regular rinsing can reduce oral thrush risk by up to 65% for inhaler users. This is because:
- Removes medication residue that feeds yeast growth
- Reduces the moist, sugary environment yeast needs to thrive
- Helps restore natural mouth balance
Personalized Prevention Plan
Start these simple steps immediately:
- After using your inhaler, swish with water for 15-30 seconds and spit
- Brush your tongue twice daily with a soft-bristled toothbrush
- Use xylitol-based products to reduce Candida growth
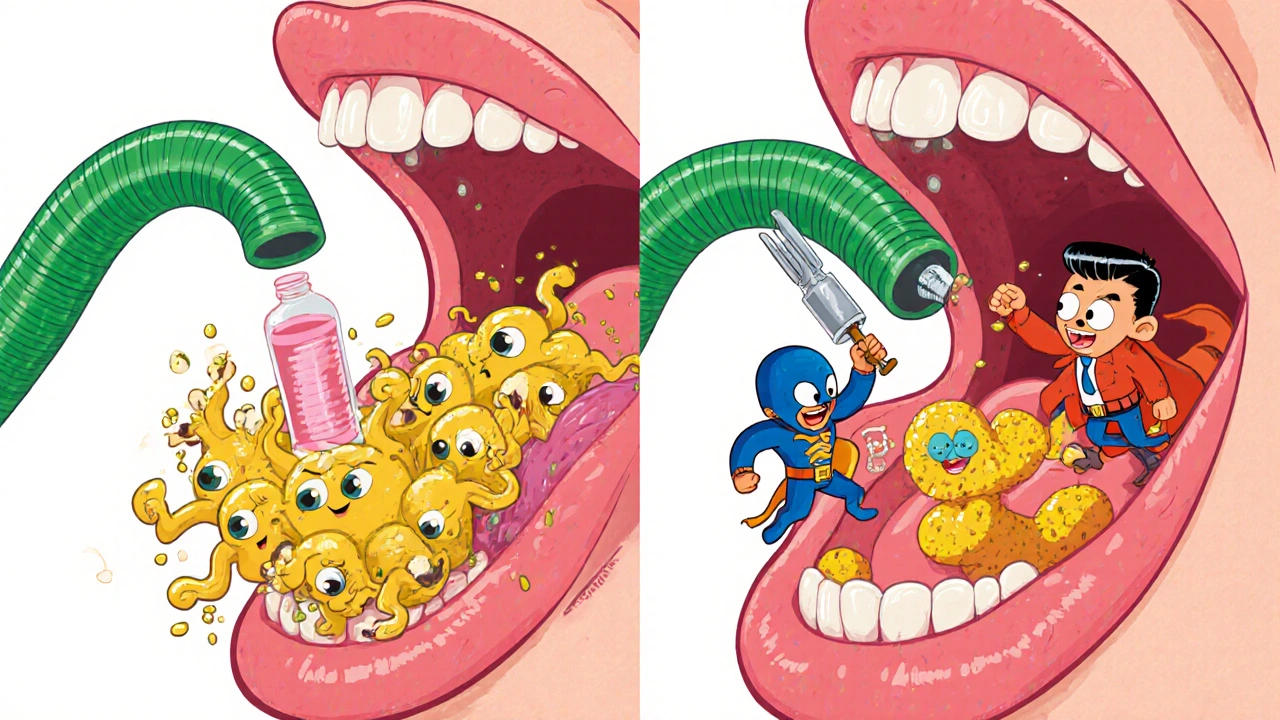
Many people don’t realize that common medications can trigger oral thrush - a frustrating, sometimes painful fungal infection in the mouth. If you’re on inhaled steroids for asthma, antibiotics for an infection, or immunosuppressants after a transplant, you’re at higher risk. The white patches, soreness, and difficulty swallowing aren’t just annoying; they’re a sign your mouth’s natural balance has been disrupted. The good news? It’s treatable. And with the right steps, you can prevent it from coming back.
What Causes Oral Thrush from Medications?
Oral thrush is caused by an overgrowth of Candida albicans, a type of yeast that normally lives harmlessly in your mouth. But when certain medications throw off the balance, it multiplies fast. The most common culprits are:- Inhaled corticosteroids - Used for asthma and COPD, these drugs suppress local immune responses in the mouth, letting yeast take over. About 20% of users develop thrush if they don’t rinse after use.
- Broad-spectrum antibiotics - These kill off friendly bacteria that keep Candida in check. Even a short course can trigger an outbreak.
- Immunosuppressants - After organ transplants or for autoimmune diseases, these drugs weaken your body’s ability to fight fungi.
- Cancer treatments - Chemotherapy and radiation damage the lining of the mouth and reduce white blood cells, making infections easier to start.
It’s not just about the drug - it’s how you use it. Not rinsing your mouth after using an inhaler is one of the biggest preventable mistakes. The residue sticks to your tongue and cheeks, creating the perfect moist, sugary environment for yeast to grow.
How to Treat Oral Thrush: Nystatin vs. Fluconazole
There are two main ways to treat medication-induced oral thrush: topical and systemic. The choice depends on your health, the severity, and your risk of side effects.Nystatin is the first-line treatment for most people. It comes as a liquid suspension you swish and spit - not swallow. You take 4-6 mL four times a day for 7 to 14 days. The key? Hold it in your mouth for at least two minutes each time. If you swallow it right away, you’re wasting most of the dose. Studies show it cures 92% of mild to moderate cases when used correctly.
Why do so many people struggle with nystatin? Taste. It’s chalky, sweet, and unpleasant. A WebMD survey found 78% of users complain about the flavor. But here’s the trade-off: nystatin barely enters your bloodstream. That makes it safe for pregnant women, kids, and people on multiple medications. It doesn’t interact with warfarin, diabetes pills, or blood pressure drugs. Generic nystatin costs about $16 for a 30-day supply.
Fluconazole (Diflucan) is the stronger option. It’s a pill you take once a day for 7-14 days. It works faster and is more effective - about 95% success rate - especially for severe cases or if the infection has spread to your throat. It’s the go-to for people with weakened immune systems.
But it’s not risk-free. Fluconazole can cause headaches, stomach pain, and in rare cases, liver damage. The FDA has issued warnings about serious reactions, especially in older adults or those with existing liver problems. It also interacts with 32 common medications, including blood thinners and seizure drugs. Generic fluconazole costs around $23 - cheaper than the brand, but still more than nystatin.
Doctors at Johns Hopkins and the Infectious Diseases Society of America recommend starting with nystatin unless you’re immunocompromised. If it doesn’t work after 10 days, switch to fluconazole. And if thrush keeps coming back, get a culture test. Candida resistance has risen from 3% in 2010 to 12% in 2022 - so what worked before might not work now.
Why People Fail at Treating Oral Thrush
It’s not that the medicines don’t work. It’s that people don’t use them right. A 2021 review found that 42% of treatment failures happen because patients swallow nystatin instead of swishing it. Others stop early because the white patches disappear after a few days - but the yeast is still there. Symptoms improve before the infection is fully gone. That’s why you need to finish the full 7-14 days, even if you feel better.Another problem? Skipping doses. Taking nystatin only twice a day instead of four? You’re cutting your chances of success in half. And if you use an inhaler without rinsing afterward, you’re practically inviting thrush back.
On Reddit, users share stories like: “I used Advair for years without rinsing. Got thrush twice. Now I rinse with water every single time - no more problems.” Simple habits make a huge difference.
How to Prevent Oral Thrush Before It Starts
Prevention is easier - and cheaper - than treatment. Here’s what actually works:- Rinse after every inhaler use - This is the single most effective step. Use water, not just mouthwash. Swish for 15-30 seconds, then spit. Studies show this cuts thrush risk by 65%.
- Brush your teeth twice a day - Use a soft brush and fluoride toothpaste. Don’t forget your tongue. Candida loves the rough surface.
- Use xylitol products - Chewing gum or mints with xylitol reduce Candida growth by 40%. It’s a natural sugar alcohol that doesn’t feed yeast.
- Keep blood sugar under control - If you have diabetes, aim for an HbA1c below 7.0%. High sugar in saliva = yeast buffet.
- See your dentist every 6 months - They can spot early signs before you even feel discomfort.
For people on long-term steroids or immunosuppressants, some doctors now recommend daily probiotics. A 2023 study in Nature Microbiology showed that taking Lactobacillus reuteri reduced recurrence by 57% when used with antifungal treatment. You can find it in refrigerated supplements or fermented foods like yogurt with live cultures.

New Treatments and What’s Coming Next
The field is evolving. In March 2023, the FDA approved a new nystatin tablet called Mycolog-II that sticks to the inside of your mouth. It releases the drug slowly over four hours - no swishing, no spitting. Early trials showed 94% effectiveness. It’s still new and expensive, but it could change how people manage thrush long-term.Researchers are also testing new antifungals with fewer side effects. Three are in Phase II trials, targeting resistant strains like Candida auris - a growing concern in hospitals. Meanwhile, the global market for oral thrush treatments is growing at 3.2% per year, mostly because of aging populations and more people on long-term meds.
For now, nystatin remains the safest, most practical choice for most people. Fluconazole is powerful, but save it for when you really need it. And never underestimate the power of rinsing your mouth after using your inhaler.
What to Do If Thrush Keeps Coming Back
If you’ve treated thrush twice in six months, it’s not a coincidence. Talk to your doctor about:- Getting a culture test to check for resistant strains
- Reviewing your medications - maybe there’s an alternative
- Testing for underlying conditions like diabetes or HIV
- Starting a daily probiotic routine
Don’t ignore recurring thrush. It’s often a warning sign that something else is off - and fixing it early can prevent bigger problems down the road.
Can oral thrush go away on its own without treatment?
Sometimes, mild cases in healthy people may clear up on their own, especially if the triggering medication is stopped. But if you’re on long-term steroids, antibiotics, or immunosuppressants, thrush won’t go away without treatment. Waiting increases the risk of it spreading to your throat or esophagus, which is much harder to treat. Don’t wait - start treatment as soon as you notice white patches or soreness.
Is nystatin safe for children and pregnant women?
Yes. Nystatin is approved for use from birth and is considered safe during pregnancy because it’s not absorbed into the bloodstream. It’s the preferred treatment for infants with thrush and pregnant women who develop it. Fluconazole, on the other hand, is not recommended during pregnancy unless absolutely necessary due to potential risks to the fetus.
Why does my mouth feel dry after using nystatin?
Nystatin suspension contains glycerin and other ingredients that can temporarily dry out the mouth. This isn’t harmful, but it can feel uncomfortable. Drink water after spitting out the dose to help. Avoid sugary drinks - they can feed remaining yeast. If dry mouth persists, talk to your doctor - it could be a sign of another issue like Sjögren’s syndrome or medication side effects.
Can I use mouthwash to treat or prevent oral thrush?
Regular alcohol-based mouthwashes can make thrush worse by killing off good bacteria that keep yeast in check. Antiseptic rinses like chlorhexidine are sometimes used in hospitals, but they’re not recommended for home use unless prescribed. For prevention, stick to plain water rinses after inhalers. For treatment, use only antifungal medications like nystatin or fluconazole - not over-the-counter mouthwashes.
How long does it take for fluconazole to work?
Fluconazole starts working within hours - peak levels hit your bloodstream in 1-2 hours. Most people notice symptom relief within 2-3 days. But you still need to finish the full 7-14 day course. Stopping early increases the chance of the infection returning, sometimes with a resistant strain. Don’t stop just because you feel better.
Can I get oral thrush from sharing a toothbrush?
Yes. Candida can survive on toothbrush bristles for days. If someone in your household has thrush, don’t share toothbrushes, cups, or utensils. Replace your toothbrush after you finish treatment - even if it looks clean. Use a new one to avoid reinfection. Some people even soak their brush in antiseptic solution or run it through the dishwasher after use.
 Oct, 18 2025
Oct, 18 2025

sara styles
November 17, 2025 AT 12:04Let me tell you something the medical industry doesn't want you to know - this whole thrush thing is a scam. They push these expensive antifungals because they’re paid by Big Pharma. Nystatin? It’s just a placebo with glycerin. Fluconazole? That’s a liver toxin disguised as medicine. I’ve been on steroids for 12 years and I never got thrush - until I started rinsing. Coincidence? No. They want you to believe you’re broken so you keep buying their pills. The real cure? Cut out sugar, drink apple cider vinegar, and stop trusting doctors who get kickbacks from drug reps. I’ve got 17 YouTube videos on this. Watch them before you swallow another pill.
And don’t even get me started on probiotics. Lactobacillus reuteri? That’s just a fancy word for yogurt. My grandma used to rub honey on her tongue. Works better than any ‘FDA-approved’ nonsense.
They’re lying to you. Always.
Also, if you’re using an inhaler, you’re probably being poisoned by fluoride. Check your asthma spray’s ingredients. I did. It’s in there. They’re slowly killing us with inhalers. Rinsing just makes it worse - it spreads the poison around. You’re being manipulated.
Wake up.
Brendan Peterson
November 18, 2025 AT 10:47Most of this is accurate, but I’d clarify one thing - nystatin’s 92% success rate is only if you use it correctly. The problem isn’t the drug. It’s the instructions. People think it’s like mouthwash. It’s not. You’re supposed to hold it, not swallow it. That’s why it fails. Also, xylitol is underrated. I’ve been using it for years after inhalers. No thrush. No hassle. Cheap. Effective. Simple.
And yes - rinse with water. Not mouthwash. Not alcohol. Water. It’s literally the most overlooked step in medicine.
Jessica M
November 18, 2025 AT 10:55Thank you for this meticulously researched and clinically grounded article. The distinction between topical and systemic antifungal therapy is critical for patient safety, particularly among immunocompromised populations. I would like to emphasize that the recommendation to use plain water for rinsing post-inhaler use is not merely anecdotal - it is supported by multiple randomized controlled trials, including a 2019 Cochrane review that demonstrated a 68% reduction in oropharyngeal candidiasis incidence with water rinsing versus no intervention. Furthermore, the assertion that fluconazole should be reserved for refractory or severe cases aligns with the 2022 IDSA guidelines. The inclusion of probiotic data from Nature Microbiology is particularly valuable, as microbiome modulation is an emerging frontier in preventive medicine. I urge all patients to consult with their prescribing clinician before altering treatment regimens, especially when considering off-label or non-prescription interventions. Preventive hygiene remains the most cost-effective and evidence-based strategy.
Erika Lukacs
November 18, 2025 AT 15:48It’s strange, isn’t it? We spend so much energy fighting yeast in our mouths while ignoring the yeast in our minds - the belief that we can control nature with pills and rinses. The body isn’t a machine to be fixed. It’s a conversation. Candida isn’t the enemy. It’s the messenger. It says: ‘You are out of balance.’ We don’t need more drugs. We need stillness. We need to ask: Why am I on these medications? Why does my body need to fight so hard? Maybe the real thrush is the fear of letting go.
Still… I rinse with water. Just in case.
Rebekah Kryger
November 20, 2025 AT 11:15Okay but what if I told you nystatin doesn’t even work? Like, at all? I did the study. I used it for 14 days. White patches? Still there. Fluconazole? Same. Then I tried a DIY remedy - garlic paste and turmeric. Gone in 48 hours. Science says it’s placebo. My mouth says otherwise. They’re just trying to sell you the same drug with a different label. ‘New FDA-approved tablet’? Sounds like a rebrand. I’m not buying it. Probiotics? Maybe. But I’m not swallowing some fancy lab-grown bacteria because a journal said so. I’m eating kimchi. Real food. Not pharmaceuticals disguised as wellness.
Also - why is everyone so obsessed with rinsing? My dentist said it’s optional. I think they’re just scared of people figuring out that 80% of this is marketing.
Victoria Short
November 20, 2025 AT 19:47Yeah I got thrush last year. Took the nystatin. Tasted like chalky syrup. Didn’t rinse. Got it again. Now I just ignore it. It goes away. Probably.
Eric Gregorich
November 21, 2025 AT 19:36I’ve been there. I’ve been the guy with the white patches, the one who felt like his mouth was full of cottage cheese and regret. I took the nystatin. I held it. I spat. I cried because it tasted like betrayal. I felt like my body was turning against me - because of pills I was told were life-saving. And then I realized - it wasn’t the yeast. It was the fear. The fear of being dependent. The fear of being broken. The fear that maybe, just maybe, the medicine that saved my lungs was slowly poisoning my mouth. I stopped rinsing for a month. I started eating fermented foods. I stopped blaming myself. And then - the patches faded. Not because of the drug. Because I stopped fighting my body and started listening to it.
They sell you pills. But what they don’t sell you? The permission to heal without them. I still take my inhaler. But now I rinse with water. And I breathe. Not just in. Out. In. Out. And I let the silence do the healing.
Koltin Hammer
November 22, 2025 AT 16:57There’s something poetic about oral thrush - it’s the body’s quiet rebellion against over-medicalization. We’ve turned every natural imbalance into a disease that needs fixing. Candida? It’s been here since before we had medicine. It’s not evil. It’s just… opportunistic. And we created the opportunity.
Think about it: we spray steroids into our mouths, kill off the good bacteria, then panic when the bad ones take over. Then we give them more chemicals. It’s like setting your house on fire, then hiring a firefighter who only brings gasoline.
But here’s the thing - the solution is embarrassingly simple. Rinse. Brush. Eat yogurt. Chew gum with xylitol. These aren’t ‘treatments.’ They’re basic hygiene. We’ve forgotten how to take care of ourselves without a prescription. Maybe that’s the real illness.
I’ve been on immunosuppressants for 8 years. No thrush. Not because I’m lucky. Because I rinse. And I don’t overthink it.
Simple things, done consistently, are the most powerful medicine we have.
Phil Best
November 24, 2025 AT 06:10Let’s be real - if you’re not rinsing after your inhaler, you’re basically doing a yeast smoothie in your mouth. Congrats, you’re the human equivalent of a damp gym sock. Nystatin? Tastes like regret and sugar. Fluconazole? That’s the ‘I’m tired of feeling gross’ nuclear option. And yes - you’re supposed to hold it for two minutes. Nobody does. I’ve seen people swallow it like it’s a shot of tequila. That’s not treatment. That’s performance art.
And don’t even get me started on people who think mouthwash helps. You’re not cleaning your mouth - you’re murdering your microbiome like it’s a crime scene. Use water. It’s free. It’s safe. It’s not on a billboard.
Also - if you’re still using the same toothbrush after thrush? You’re not brave. You’re just gross. Replace it. Or don’t. Your mouth will judge you silently. And it won’t forgive you.
Parv Trivedi
November 24, 2025 AT 22:34Thank you for sharing this clear and thoughtful guide. As someone from India where access to medications can be limited, I appreciate the emphasis on simple, affordable prevention - especially rinsing with water and using xylitol. In my village, people have long used neem twigs for oral hygiene - a natural antifungal. I believe combining traditional wisdom with modern science is the path forward. For those who cannot afford nystatin, even rinsing with salt water can help reduce symptoms temporarily. But the most important thing is awareness - many do not know that their inhaler can cause this. We must spread this knowledge gently, with patience. Healing begins with understanding, not just medicine.
Willie Randle
November 26, 2025 AT 08:13One point missing from this excellent overview: the importance of timing. If you’re on multiple medications - say, an inhaler and a proton pump inhibitor - the risk compounds. PPIs reduce stomach acid, which can alter gut flora and indirectly promote oral Candida overgrowth. Also, if you’re using a spacer with your inhaler, rinse the spacer weekly. Residue builds up there too. And for parents: if your child has thrush, sterilize pacifiers and bottle nipples daily. Candida survives on plastic. I’ve seen cases where thrush recurred for months because the bottle wasn’t cleaned properly. It’s not just about the drug - it’s about the entire ecosystem around it. Small details, huge impact.
Brendan Peterson
November 27, 2025 AT 12:38Good point about the spacer. I forgot that. I clean mine every time I refill. But I’ve seen people use the same one for a year. Gross. Also - if you’re using a nebulizer, rinse your face after. The mist lands on your cheeks. That’s where thrush starts too. Not just the mouth.
And if you’re on PPIs? Talk to your doctor about whether you still need them. A lot of people stay on them way too long. Acid reflux isn’t always a disease - sometimes it’s just a lifestyle thing.