Renal Opioid Dosing Calculator
Opioid Safety Guidelines
Use with opioid tolerance
Monitor for QT prolongation
Avoid in all stages of kidney disease
Patient Assessment
Dosing Results
Select parameters to see results
Managing pain in patients with kidney failure isn’t just harder-it’s riskier. When the kidneys can’t filter properly, many common pain medications build up to dangerous levels. Opioids, often used for chronic pain, become a minefield in advanced kidney disease. Some opioids turn into toxic metabolites that cause seizures, confusion, or even respiratory arrest. Others are cleared mostly by the liver and stay safe. The difference between relief and harm often comes down to choosing the right drug and the right dose.
Why Opioids Are Risky in Kidney Failure
Most opioids are broken down in the liver and then filtered out by the kidneys. In someone with a glomerular filtration rate (GFR) below 30 mL/min, that cleanup process slows down dramatically. What’s worse, some opioids don’t just linger-they transform into active toxins. Morphine, for example, turns into morphine-3-glucuronide. That metabolite doesn’t help with pain. Instead, it causes muscle twitching, hallucinations, and seizures. Codeine becomes codeine-6-glucuronide, which has the same neurotoxic effect. These aren’t side effects you can ignore. They’re medical emergencies.
Meperidine (pethidine) is even more dangerous. Its metabolite, normeperidine, builds up quickly and can trigger seizures at levels as low as 0.6 mg/L. That’s why it’s banned in all stages of kidney disease, including dialysis. Even if a patient seems stable, giving them meperidine is like lighting a fuse.
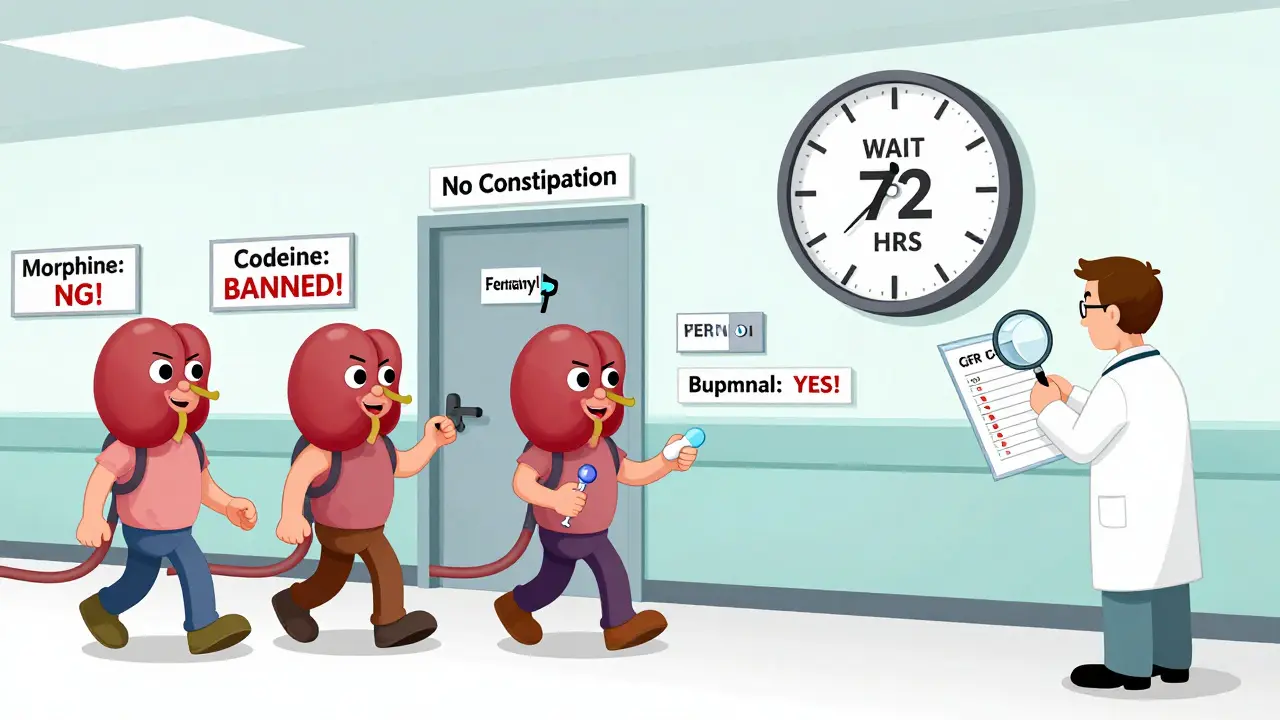
Safe Opioid Choices for Kidney Patients
Not all opioids are created equal. The safest options for kidney failure are those that are mostly processed by the liver and cleared in small amounts by the kidneys. Two stand out: fentanyl and buprenorphine.
Fentanyl is 93% metabolized by the liver. Only 7% leaves the body through the kidneys. That makes it one of the few opioids you can use safely even in end-stage renal disease. Studies show no dangerous buildup in patients with GFR under 10 mL/min. It’s often given as a patch-transdermal delivery means steady blood levels, fewer spikes, and less risk of overdose. But here’s the catch: never start a fentanyl patch in someone who’s never taken opioids before. The risk of fatal respiratory depression is too high. It’s only for patients already tolerant to opioids.
Buprenorphine is another top choice. About 30% of it is cleared by the kidneys, but because it’s so strongly bound to liver enzymes, it doesn’t accumulate. Multiple studies confirm it’s safe in dialysis patients without dose changes. It’s also less likely to cause respiratory depression than other opioids, making it safer for older or frail patients. The only warning? It can prolong the QT interval on an ECG. So if the patient has heart rhythm issues, monitor them closely.
Opioids to Avoid at All Costs
Some opioids should never touch a kidney patient. The Kidney Disease: Improving Global Outcomes (KDIGO) guidelines list four as absolute no-gos:
- Morphine - Metabolites accumulate, causing neurotoxicity
- Codeine - Converts to toxic metabolites; also ineffective in poor CYP2D6 metabolizers
- Meperidine - High risk of seizures even at low doses
- Propoxyphene - Withdrawn from most markets but still found in some regions; highly toxic in renal failure
Hydromorphone is tricky. While the parent drug is mostly liver-metabolized, its metabolite-hydromorphone-3-glucuronide-builds up in non-dialysis patients. One study showed a 37% higher risk of neurotoxicity compared to those on dialysis. So if you must use it, only do so in patients receiving regular hemodialysis and watch for confusion or tremors.
Oxycodone is sometimes used, but with caution. About 45% of its metabolites are cleared by the kidneys. For patients with GFR under 30 mL/min, daily doses should not exceed 20 mg. Still, there’s no strong consensus on its safety, so many nephrologists avoid it unless no other option exists.

Dosing Adjustments Based on Kidney Function
Even safe opioids need dose changes in kidney failure. Here’s what works in practice:
- GFR >50 mL/min: Use standard doses for fentanyl, methadone, and buprenorphine.
- GFR 10-50 mL/min: Reduce morphine to 50-75% of usual dose. Fentanyl can stay at 75-100%. Methadone and buprenorphine don’t need adjustment.
- GFR <10 mL/min (including dialysis): Morphine should be cut to 25% of normal. Methadone to 50-75%. Fentanyl to 50%. Buprenorphine unchanged.
Start low. Go slow. Always begin with half the usual dose in advanced kidney disease. Wait 48-72 hours before increasing. Pain relief isn’t urgent-it’s a marathon, not a sprint. Rushing doses leads to overdose. And remember: dialysis doesn’t remove fentanyl or buprenorphine effectively. Don’t give extra doses after dialysis unless the patient is in severe pain and you’ve ruled out other causes.
Special Cases: Dialysis Patients and Transdermal Patches
Patients on hemodialysis have unique needs. Fentanyl patches are safe between sessions, but never apply one right before or during dialysis. The process can alter drug absorption unpredictably. Buprenorphine patches are even better here-they’re stable across dialysis cycles.
For acute pain in dialysis patients, intravenous morphine is sometimes used-but only in tiny amounts (1-2 mg) and only if no alternatives exist. The risk of metabolite buildup is still there, even during dialysis. Most nephrologists prefer to avoid it entirely.
Transdermal delivery (patches) is preferred for chronic pain because it avoids first-pass metabolism and gives steady levels. But patches aren’t for everyone. Skin irritation, heat exposure, or poor circulation can affect absorption. Always check the patch site and monitor for signs of toxicity.
What About Non-Opioid Options?
Opioids aren’t the only tool. In fact, they shouldn’t be the first. For neuropathic pain, gabapentin and pregabalin are common-but they need heavy dose reductions. Gabapentin should be limited to 200-700 mg once daily in GFR <30 mL/min. Pregabalin requires longer intervals between doses. Both can cause dizziness and falls in elderly patients.
Tricyclic antidepressants like nortriptyline carry heart risks in kidney patients. Serum levels above 100 ng/mL triple the chance of dangerous arrhythmias. They’re not off-limits, but they demand blood tests and ECGs.
For opioid-induced constipation-a problem in 40-80% of patients-naldemedine is the best choice. Unlike other laxatives for this issue, it doesn’t need dose adjustment in kidney failure. Standard dose: 0.2 mg daily. It works without affecting pain relief.
Real-World Challenges and Gaps
Here’s the hard truth: 88% of opioid package inserts don’t mention kidney dosing. Doctors are left guessing. That’s why only 12% of kidney patients get guideline-approved opioid care. Many are left in pain because providers fear toxicity.
Some hospitals have fixed this by adding clinical decision tools into their electronic records. Kaiser Permanente reduced inappropriate opioid prescriptions by 47% in CKD patients between 2018 and 2022 by flagging unsafe choices before they’re written.
Research is catching up. The NIDDK’s PAIN-CKD study, launched in 2021, is tracking 1,200 patients over five years to find which regimens work best long-term. Early signs point to buprenorphine and fentanyl as top performers. Future guidelines may even use genetic testing-CYP2D6 poor metabolizers are over three times more likely to have morphine toxicity in kidney failure.
Final Takeaways
When treating pain in kidney failure:
- Start with non-opioid options whenever possible.
- If opioids are needed, choose fentanyl or buprenorphine.
- Avoid morphine, codeine, meperidine, and propoxyphene at all costs.
- Reduce doses by 50% or more in advanced kidney disease.
- Use transdermal patches for stable, long-term control.
- Monitor for neurotoxicity: tremors, confusion, myoclonus.
- Always check for drug interactions and cardiac risks.
Pain is real. But so is the risk. The goal isn’t to eliminate opioids-it’s to use them wisely. The right drug, at the right dose, with careful monitoring, can restore quality of life without putting life at risk.
Which opioids are safest for patients with kidney failure?
Fentanyl and buprenorphine are the safest choices. Both are primarily metabolized by the liver, with minimal kidney clearance. Fentanyl is ideal for chronic pain via patch, and buprenorphine works well even during dialysis. Neither requires dose reduction in advanced kidney disease, unlike morphine or oxycodone.
Can you use morphine in kidney failure?
No, morphine is contraindicated in moderate to severe kidney failure. Its metabolite, morphine-3-glucuronide, accumulates and causes neurotoxicity-leading to seizures, muscle spasms, and confusion. Even reduced doses carry risk. Avoid it entirely in GFR under 50 mL/min.
Do I need to adjust opioid doses for dialysis patients?
Yes, but not for all opioids. Fentanyl and buprenorphine don’t need dose changes because dialysis doesn’t remove them effectively. Morphine and hydromorphone still require dose reductions because their metabolites aren’t fully cleared during dialysis. Always start at half the usual dose and titrate slowly.
Why is meperidine banned in kidney disease?
Meperidine breaks down into normeperidine, a neurotoxic metabolite that builds up quickly in kidney failure. At levels above 0.6 mg/L, it causes seizures and can be fatal. Even a single dose can be dangerous in patients with GFR under 30 mL/min. It’s strictly prohibited in all stages of chronic kidney disease.
How do you treat constipation from opioids in kidney patients?
Naldemedine is the preferred treatment. Unlike other laxatives for opioid-induced constipation, it doesn’t require dose adjustment in kidney failure or dialysis. Standard dose is 0.2 mg once daily. It works locally in the gut without interfering with pain relief or causing systemic side effects.
What should I do if a kidney patient develops confusion or twitching on opioids?
Stop the opioid immediately. Neurotoxicity from metabolite buildup is likely. Switch to a safer agent like buprenorphine or fentanyl. Supportive care includes hydration, electrolyte correction, and monitoring for seizures. In severe cases, consider naloxone-but only if respiratory depression is present, since neurotoxicity doesn’t always respond to it.
 Dec, 25 2025
Dec, 25 2025

roger dalomba
December 27, 2025 AT 04:40Fentanyl patches for kidney patients? Sure, if you’re okay with turning someone into a zombie who can’t remember their own name. At least morphine gives you a good hallucination before the seizure. 😏
Brittany Fuhs
December 29, 2025 AT 03:58It’s disgusting how we let pharmaceutical companies push dangerous drugs on vulnerable people. The FDA should’ve banned these opioids decades ago. This isn’t medicine-it’s corporate negligence wrapped in a white coat.
Peter sullen
December 30, 2025 AT 01:11It is imperative to underscore, with the utmost clinical precision, that the pharmacokinetic profile of fentanyl-particularly its hepatic metabolism via CYP3A4, coupled with negligible renal excretion (<7%)-renders it the preeminent opioid agent in the context of advanced chronic kidney disease (CKD), especially when GFR is <10 mL/min/1.73m². Moreover, the transdermal delivery system affords a steady-state plasma concentration, thereby minimizing the risk of supratherapeutic peaks that precipitate respiratory depression. Buprenorphine, likewise, demonstrates a high affinity for mu-opioid receptors with a ceiling effect on respiratory suppression, making it an ideal candidate for frail, elderly, or polypharmacy patients with concomitant cardiac arrhythmias. However, QT prolongation remains a critical consideration requiring baseline ECG and serial monitoring.
Steven Destiny
December 30, 2025 AT 20:00Stop coddling patients with kidney failure. If they can’t handle pain meds without turning into a seizure-prone mess, maybe they shouldn’t have waited until stage 5 to get help. This isn’t rocket science-avoid the bad ones, use the safe ones, and stop acting like every patient needs a VIP pain pass.
Fabio Raphael
December 31, 2025 AT 01:01I’ve seen patients on dialysis who were in agony for months because doctors were too scared to prescribe anything. Then someone finally gave them a low-dose buprenorphine patch-and they cried because they could sleep again. It’s not about risk. It’s about balance. We’re not just treating labs-we’re treating people who’ve lost their quality of life. Please don’t let fear silence compassion.
Amy Lesleighter (Wales)
January 1, 2026 AT 07:10Just use buprenorphine. It works. It’s safe. It doesn’t make you hallucinate. Stop overcomplicating it. People are suffering.
Rajni Jain
January 2, 2026 AT 03:14Thank you for writing this. My dad’s on dialysis and they kept giving him morphine until he started twitching like he was having a bad trip. We switched to fentanyl patch and he finally smiled again. I wish more doctors knew this.
Natasha Sandra
January 4, 2026 AT 00:54So happy to see someone finally talking about this! 🙌 Buprenorphine is a game changer. My aunt’s been on it for 2 years now and she’s back to gardening and baking pies 🥧❤️ Let’s spread the word! #KidneySafePainRelief