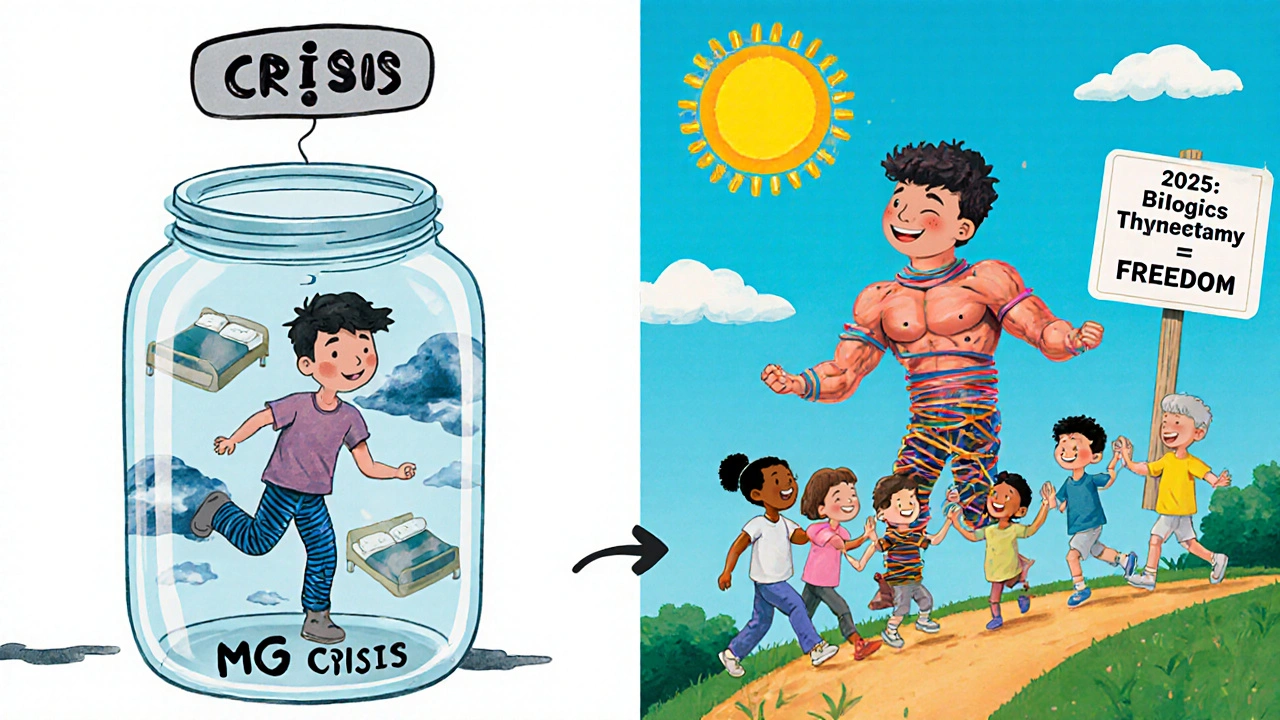
Myasthenia gravis (MG) isn’t just muscle weakness. It’s your body turning against itself-attacking the very connection between nerves and muscles. Imagine trying to lift your eyelid, chew food, or even breathe, and your muscles suddenly giving out. Then, after resting, they come back. That’s MG. It’s rare, unpredictable, and until recently, hard to treat beyond temporary fixes. But as of 2025, the treatment landscape has changed dramatically. We’re no longer just masking symptoms. We’re targeting the root cause.
How Myasthenia Gravis Breaks the Nerve-Muscle Connection
Your nerves send signals to muscles using a chemical called acetylcholine. In MG, your immune system makes antibodies that block or destroy the receptors on muscle cells that receive this signal. Without that connection, muscles don’t get the message to contract. About 85% of people with generalized MG have antibodies against the acetylcholine receptor (AChR). Another 5-8% have antibodies against MuSK, a different protein involved in the same process. Around 1 in 10 have no detectable antibodies-called seronegative MG-but still have the same symptoms.
This isn’t just random. The thymus gland, located behind the breastbone, plays a key role. In many MG patients, it’s enlarged or even contains a tumor (thymoma). For decades, doctors didn’t know why. Now we know: the thymus is where these rogue antibodies are often made. Removing it isn’t just a surgery-it’s part of the treatment.
First-Line Treatment: Symptom Relief and Immune Suppression
Almost everyone with MG starts with pyridostigmine (Mestinon). It doesn’t fix the immune problem. Instead, it slows down the breakdown of acetylcholine, giving more time for the remaining signals to work. Doses range from 60 to 120 mg every 3 to 6 hours. Side effects? Up to half of patients get stomach cramps, diarrhea, or excessive salivation. But for many, it’s the difference between managing daily life and being housebound.
When symptoms are more than mild, corticosteroids like prednisone are added. They work fast-70-80% of patients improve within weeks. But the cost is high. Weight gain hits 65% of users. Osteoporosis develops in 1 in 4 after a year. Diabetes appears in 15-20%. That’s why doctors try to lower the dose as soon as possible.
Long-term immune control usually means switching to drugs like azathioprine, mycophenolate, or cyclosporine. Azathioprine takes 6 to 18 months to work but has fewer long-term side effects than steroids. Mycophenolate is easier to tolerate, but 3 in 10 people get nausea or diarrhea. Cyclosporine works well-90% respond-but it can damage kidneys and raise blood pressure. These aren’t perfect, but they’re affordable: $500 to $2,000 a year.
Thymectomy: Removing the Source of the Attack
If you’re between 18 and 65, have AChR-positive MG, and no major health issues, thymectomy is now standard care. The 2016 MGTX trial proved it: over three years, patients who had the surgery needed 56% less steroid and had 67% fewer hospital stays than those on medication alone.
The surgery can be done through a traditional open chest cut or minimally invasive methods like robotic or video-assisted thoracoscopy. Open surgery has the most proven long-term results-35-40% of patients achieve complete, stable remission after five years. Minimally invasive options are less painful and heal faster, but we don’t yet know if they offer the same lasting benefit.
Even after surgery, most people still need medication. But many find they can reduce doses significantly. One patient I spoke with said, “I went from 60 mg of prednisone to 5 mg. I can finally walk without stopping every 10 minutes.”

Targeted Biologics: The New Generation of MG Drugs
Since 2017, a wave of new drugs has transformed MG care. These aren’t broad immune suppressants. They’re precision tools designed to block specific parts of the autoimmune attack.
Complement inhibitors like eculizumab and ravulizumab stop the immune system from destroying muscle receptors. They’re powerful-88% of patients improve, and over half reach minimal manifestation status. But they require IV infusions every 2 weeks, cost $500,000-$600,000 a year, and you must get vaccinated against meningitis first. They work best for AChR-positive MG.
FcRn inhibitors are the game-changers. Drugs like efgartigimod, rozanolixizumab, nipocalimab, and batoclimab lower the level of all IgG antibodies-including the bad ones. They work fast: improvement in 1-2 weeks. They’re effective across antibody types, even in seronegative MG. Rozanolixizumab is given as a weekly shot under the skin. Nipocalimab, approved in April 2025, reduces IgG by 70-80%. These cost $300,000-$400,000 a year, but many patients report life-changing results. One Reddit user wrote: “I went from needing help to stand up to hiking 3 miles in a week. No more IVs, just a quick injection.”
B-cell therapy like rituximab is especially helpful for MuSK-MG, with 80% response rates. But for AChR-positive patients, it’s less reliable-only 50-60% improve. It’s cheaper than biologics ($10,000-$15,000 per course) but takes months to work.
Fast-Acting Options for Crises
When MG flares badly-like when breathing becomes difficult-doctors use rapid interventions. Plasmapheresis removes antibodies directly from the blood. Five sessions over 7-10 days can clear 60-80% of harmful antibodies. IVIG (intravenous immunoglobulin) floods the system with healthy antibodies to neutralize the bad ones. Both work in days, not weeks. But the relief lasts only weeks to months. These are rescue tools, not long-term solutions.
Choosing the Right Treatment: It’s Personal
There’s no one-size-fits-all. Your treatment plan depends on:
- Your antibody status (AChR, MuSK, or seronegative)
- How severe your symptoms are
- Your age and other health conditions
- What side effects you can tolerate
- Insurance coverage and cost
Most patients start with pyridostigmine and prednisone. If that’s not enough after 3-6 months, they move to azathioprine or mycophenolate. If symptoms remain uncontrolled-or if they’re severe from the start-doctors jump to biologics. Thymectomy is recommended within the first year for eligible patients.
For MuSK-MG, rituximab is often tried earlier. For seronegative MG, FcRn inhibitors like efgartigimod are now the best option, thanks to the 2024 ADAPT SERON study showing 68% response rates.
What’s Next? The Future of MG Treatment
The field is moving fast. In 2025, we saw the approval of nipocalimab and the release of strong data for batoclimab. Phase 1 trials of CAR T-cell therapy are showing 60% remission in the toughest cases. Researchers are also testing agrin mimetics-drugs that protect the nerve-muscle junction itself.
But the biggest hurdle isn’t science-it’s access. In the U.S., 40% of eligible patients can’t get insurance approval for biologics. The process can take 3-6 months. Many patients delay treatment, risking permanent muscle damage.
Doctors are also realizing that current tests don’t catch early changes. Antibody levels don’t drop until months after symptoms improve. New tools like quantitative muscle testing and IgG4-specific assays are coming, and by 2026, they could let us adjust treatment before a crisis hits.
Living With MG Today
MG isn’t cured yet. But it’s no longer a death sentence or a life of constant decline. Most people can live full, active lives. The key is early, accurate diagnosis and a tailored treatment plan.
Support matters too. The Myasthenia Gravis Foundation of America offers a 24/7 nurse hotline and 147 local support groups. Patients who connect with others report better mental health and more confidence managing their care.
One thing is clear: the days of just waiting for symptoms to pass are over. We now have tools to stop the attack, protect the junction, and restore function. If you or someone you know has MG, ask about antibody testing, thymectomy eligibility, and biologic options. The treatment landscape has changed-and it’s never been better.
Can myasthenia gravis be cured?
There is no cure yet, but many people achieve long-term remission. About 35-40% of patients who have a thymectomy reach complete, stable remission after five years. Others reach minimal manifestation status-where symptoms are barely noticeable-with the right combination of medications. Some may eventually stop all treatment under medical supervision.
How long do FcRn inhibitors take to work?
FcRn inhibitors like efgartigimod and rozanolixizumab start working in 1 to 2 weeks. Most patients notice improvement in strength, speech, or swallowing within 10 days. This is much faster than traditional immunosuppressants, which can take 3 to 6 months to show full effect.
Is thymectomy worth it if I don’t have a thymoma?
Yes. Even without a tumor, removing the thymus reduces antibody production and improves long-term outcomes. The MGTX trial showed a 56% reduction in steroid use and a 67% drop in hospitalizations over three years. It’s now standard for AChR-positive patients aged 18-65, regardless of tumor presence.
Are these new biologic drugs safe?
They’re safer than long-term steroids or cyclosporine. The biggest risk with complement inhibitors is meningococcal infection-so vaccination is required. FcRn inhibitors have fewer serious side effects, mostly mild headaches or injection site reactions. They don’t cause diabetes, bone loss, or kidney damage like older drugs. But they’re still new, and long-term data beyond 5 years is limited.
Why is myasthenia gravis harder to treat in older adults?
Older patients often have other health problems-like heart disease, kidney issues, or osteoporosis-that make steroids and immunosuppressants riskier. Thymectomy is usually avoided after 65 due to surgical risks. Newer biologics are better tolerated, but dosing and monitoring need to be adjusted. Research is now focusing on geriatric-specific protocols to improve outcomes in this growing group.
Can I get pregnant if I have myasthenia gravis?
Yes, but planning is critical. Pregnancy can worsen MG symptoms, especially in the first trimester and postpartum. FcRn inhibitors are not recommended during pregnancy because they can cross the placenta and affect the baby’s immune system. Pyridostigmine and azathioprine are considered safer options. Always work with a neurologist and obstetrician experienced in MG before conceiving.
How do I know if my treatment is working?
Doctors use standardized scores like the MG-ADL (Myasthenia Gravis Activities of Daily Living) and QMG (Quantitative Myasthenia Gravis). These track symptoms like eyelid drooping, speech, swallowing, and walking. Improvement is measured over weeks to months-not just how you feel. Antibody levels don’t change quickly, so don’t rely on them alone. Regular testing every 4-12 weeks is standard.
What should I do if my insurance denies a biologic?
Appeal immediately. Many insurers require a prior authorization process that can take months. Work with your neurologist to submit detailed clinical notes showing failed trials of other drugs. The Myasthenia Gravis Foundation of America has patient advocates who help with appeals. Some drug manufacturers also offer free medication programs during the approval process.
 Nov, 23 2025
Nov, 23 2025

Neoma Geoghegan
November 24, 2025 AT 05:07FcRn inhibitors changed my life. No more IVs, just a quick shot. I’m hiking again. This isn’t hope-it’s science.
Bartholemy Tuite
November 26, 2025 AT 04:15Man, I read this whole thing and honestly? I thought MG was just one of those rare diseases people forget about. Turns out we got actual breakthroughs now. Thymectomy isn’t just some old-school surgery anymore-it’s a game changer. And don’t even get me started on rozanolixizumab. Weekly shot? That’s like getting your life back on a subscription plan. I’m telling my cousin who’s got it to stop waiting and push for antibody testing. No more ‘wait and see’ bullshit.
Sam Jepsen
November 27, 2025 AT 17:56Just wanted to say thank you for writing this. My sister was diagnosed last year and we were drowning in info. This is the first thing that actually made sense. The part about FcRn inhibitors working in 1-2 weeks? That’s the kind of hope people need. I’m sharing this with every MG support group I can find. You did good.
Yvonne Franklin
November 29, 2025 AT 04:36Thymectomy success rates are higher than most think. 35-40% remission at 5 years isn’t magic-it’s measurable. And for AChR+ patients under 65, it’s standard of care now. Skip the hesitation. Get the scan. Get the consult. Don’t wait for it to get worse.
Michael Fitzpatrick
November 29, 2025 AT 20:19I’ve been following MG research for years and honestly, I never thought we’d get here. The fact that we can now target IgG antibodies directly without wiping out the whole immune system? That’s huge. I remember when the only options were steroids and hope. Now we’ve got precision tools. I know the cost is insane but… I feel like we’re finally moving past survival mode into living mode. Even if it’s slow, it’s real.
Shawn Daughhetee
November 30, 2025 AT 17:56My uncle had MG and they gave him prednisone and told him to tough it out. He lost 40 pounds and couldn’t lift his head for months. I wish someone had told us about thymectomy or FcRn stuff back then. This article feels like a lifeline to people still stuck in the dark ages of treatment. Thank you for writing it.
Miruna Alexandru
December 2, 2025 AT 09:34Let’s not romanticize the biologics. Yes, they work. But $400k/year? And you need to be AChR-positive to even qualify for the best ones? The fact that seronegative patients are only now getting decent options after decades of being ignored speaks to systemic neglect. Also, ‘minimal manifestation status’ is just medical euphemism for ‘still disabled but less visibly so.’ Don’t call this a cure. Call it progress with a price tag.
Justin Daniel
December 4, 2025 AT 01:59Hey Miruna, you’re not wrong about the cost-but you’re also missing the bigger picture. For the first time ever, people with MG have a shot at not just surviving, but *living*. Yeah, insurance fights are brutal. But the fact that we’re even having this conversation-that these drugs exist-is a win. I’ve seen people go from wheelchairs to walking their kids to school. That’s not a price tag. That’s dignity. Let’s fight for access, not downplay the breakthrough.
Mark Williams
December 4, 2025 AT 15:21Quick note on the ADAPT SERON study: 68% response in seronegative MG with efgartigimod is huge because prior to this, we had zero targeted options. That’s not just data-it’s a paradigm shift. Also, CAR T-cell trials are promising but still Phase 1. Don’t get ahead of the data. But yeah, the trajectory is insane. We’re 5 years from a cure, maybe 10.
David Cunningham
December 6, 2025 AT 11:12My mate in Perth got on rozanolixizumab last year. He went from needing help to stand up to riding his bike to work. No drama, no IVs. Just a little shot and boom-he’s back. This isn’t sci-fi. It’s happening right now. If you’re reading this and you’ve got MG, talk to your neurologist. Don’t wait for someone else to fix it.
luke young
December 7, 2025 AT 10:54Just wanted to add-support groups matter more than meds sometimes. I joined one after my diagnosis and realized I wasn’t broken. Just fighting a weird disease. The MGFA hotline saved me more than one night. You’re not alone. Seriously.