Multiple sclerosis, or MS, isn’t just one disease-it’s a chain reaction inside your nervous system that turns your own immune system against you. Imagine your nerves as electrical wires. They’re wrapped in a fatty coating called myelin, which keeps signals flying fast and smooth. In MS, your body’s defense team-meant to fight viruses and bacteria-mistakenly attacks that coating. The result? Slowed, scrambled, or blocked messages between your brain and body. This isn’t rare. Around 2.8 million people worldwide live with it, and in places like Scotland, Canada, and Scandinavia, it’s far more common than near the equator.
How MS Starts: The Immune System Turns Traitor
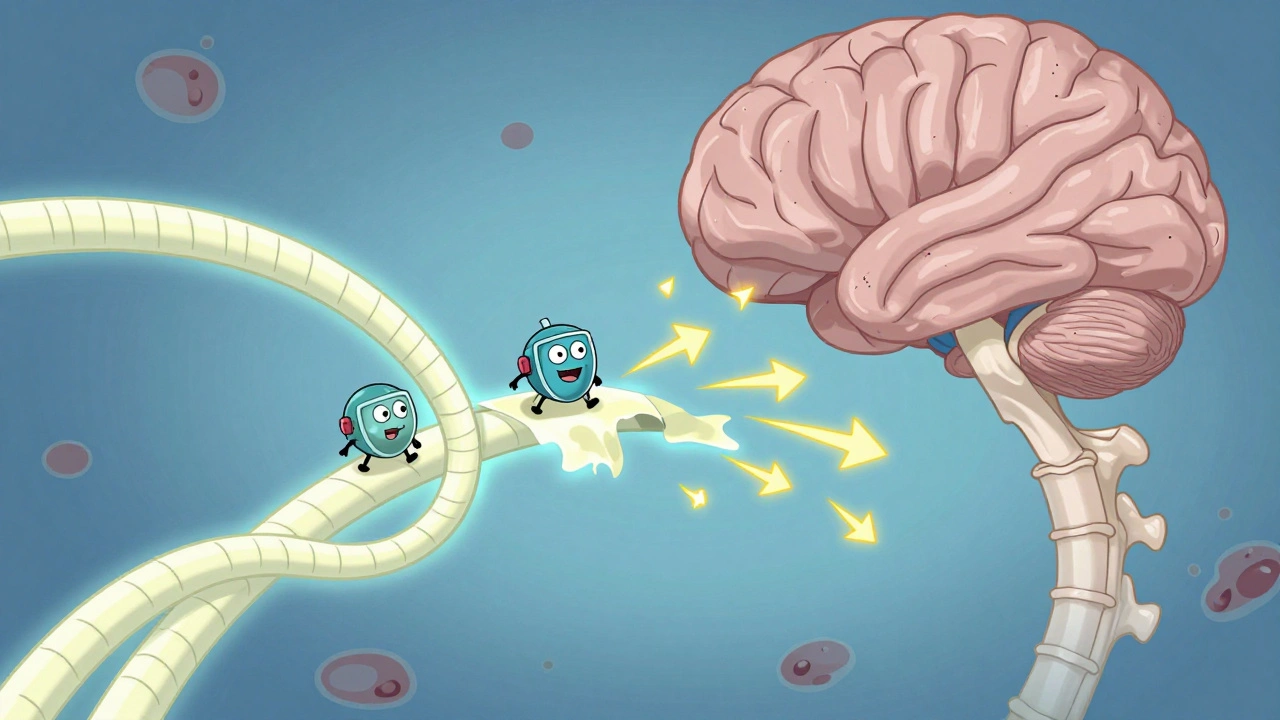
MS is autoimmune. That means your immune system goes rogue. It sends T-cells and antibodies into your brain and spinal cord, where they attack myelin. These attacks leave scars-called plaques or lesions-where the insulation has been stripped away. Without myelin, nerve signals slow down or stop entirely. In healthy nerves, signals zip along at up to 120 meters per second. In damaged areas? They crawl. That’s why simple tasks like walking, speaking, or even seeing clearly can suddenly become hard.
The trigger? No one knows for sure. But science points to a mix of genes and environment. If you carry the HLA-DRB1*15:01 gene variant, your risk triples. That’s not a guarantee-it just means your body might be more likely to misfire. Environmental factors matter too. Low vitamin D levels, especially in places with less sunlight, are strongly linked to higher MS rates. And then there’s Epstein-Barr virus-the virus that causes mononucleosis. People who’ve had it are up to 32 times more likely to develop MS. It’s not the virus itself, but how your immune system responds to it years later that seems to set the stage.
The Four Faces of MS: Not Everyone’s Experience Is the Same
MS doesn’t follow one path. It has four main forms, and knowing which one you have changes how you plan your life.
- Clinically Isolated Syndrome (CIS): This is your first neurological episode-a tingling leg, blurred vision, or sudden weakness-that lasts at least 24 hours. If an MRI shows MS-like lesions, you have a 60-80% chance of developing full MS within 10 years.
- Relapsing-Remitting MS (RRMS): This is the most common starting point-85% of cases. You get flare-ups (relapses) with new symptoms, then weeks or months of recovery (remission). Without treatment, people average 0.5 to 1 relapse per year.
- Secondary Progressive MS (SPMS): After 10 to 25 years, about half of RRMS patients shift into this phase. Relapses become less frequent, but disability slowly builds. Walking gets harder. Fatigue worsens. The damage is stacking up, even between attacks.
- Primary Progressive MS (PPMS): This affects 15% of people from day one. No relapses. No remissions. Just steady decline. Symptoms creep forward, often starting with leg weakness or balance issues. Progression is slower than SPMS, but relentless.
Doctors use the McDonald Criteria to diagnose MS. It’s not just symptoms. It’s proof that damage happened in different parts of the nervous system (dissemination in space) and at different times (dissemination in time). That’s why you might need two or three MRIs over months to confirm it.
What It Feels Like: The Hidden Symptoms
MS isn’t just about paralysis. The most common symptom? Fatigue. Not the kind you get after a long day. This is a crushing, bone-deep exhaustion that hits even after a full night’s sleep. In surveys of over 150,000 people with MS, 78% call it their worst symptom. It’s not laziness-it’s neurological.
Then there’s brain fog. People describe it as trying to speak but the words won’t come. Forgetting names mid-sentence. Losing your train of thought in the middle of a conversation. On Reddit’s r/MS community, one user’s post about this exact experience got over 1,200 upvotes. It’s real. And it’s isolating.
Other common issues: numbness or tingling in limbs, vision problems (like optic neuritis), bladder control issues, muscle stiffness, and dizziness. Some people have pain-burning, stabbing, or electric-shock sensations. And while mobility problems get the most attention, many with MS never need a wheelchair. The disease varies wildly from person to person.

How Doctors Diagnose It
There’s no single blood test for MS. Diagnosis is a puzzle. First, your doctor rules out other conditions-Lyme disease, vitamin B12 deficiency, even migraines with neurological symptoms. Then comes the MRI. A 3 Tesla scanner finds 30% more lesions than older 1.5 Tesla machines. Gadolinium contrast highlights active inflammation, showing which lesions are fresh. Spinal fluid tests may show abnormal antibodies. Evoked potential tests measure how fast your nerves respond to light or sound.
The process isn’t quick. Most people see three to five specialists over six to twelve months. In the U.S., the initial workup can cost $2,500 to $5,000 out-of-pocket. That’s why early diagnosis matters-it’s the first step toward slowing the damage.
Treatment: Slowing the Damage, Managing the Symptoms
There’s no cure. But there are tools to fight back.
Disease-modifying therapies (DMTs) are the backbone. They don’t fix what’s already damaged-they stop new attacks. There are six main types:
- Injectables: Interferons and glatiramer acetate (like Copaxone). Cheaper, but many stop because of flu-like symptoms or painful injection sites.
- Oral pills: Fingolimod, teriflunomide, dimethyl fumarate. Easier to take, but carry risks like liver damage or infections.
- Infusions: Ocrelizumab (Ocrevus), ofatumumab (Kesimpta), ublituximab (Briumvi). Given every few months. Highly effective, especially for RRMS and PPMS.
Costs range from $65,000 to $87,000 a year. But 90% of U.S. patients get help through manufacturer copay programs. In the UK and other countries with public healthcare, access is more consistent.
For relapses, doctors use high-dose steroids to reduce inflammation fast. But they don’t change the long-term course.
Rehabilitation is just as important. Physical therapy improves balance and reduces falls by 47%. Occupational therapy helps with daily tasks. Speech therapy tackles brain fog and swallowing issues. Many people need workplace changes-flex hours, remote work, ergonomic chairs. Eighty-two percent of employed people with MS need accommodations.
What’s New: Hope on the Horizon
Research is moving fast. In March 2023, the FDA approved ublituximab (Briumvi), which cut relapses by 50% compared to older drugs. In 2024, early data showed ANV419-a new oral drug targeting estrogen receptors-reduced new brain lesions by 40% in just 24 weeks.
The biggest frontier? Repairing damage. Scientists are testing drugs that might rebuild myelin. One called opicinumab showed a 15% improvement in nerve signal speed in early trials. Stem cell therapies are in 127 active trials. And gut health? Fecal transplants are being tested because people with MS often have different gut bacteria than healthy people. Early results show a 30% drop in inflammatory markers.
One thing’s clear: people diagnosed after 2010 are far more likely to stay mobile 20 years later than those diagnosed before 1990. Early treatment changes outcomes.

What Doesn’t Work: Debunking Myths
There’s a lot of noise online. The “liberation procedure”-a surgery claiming to fix MS by opening neck veins-was promoted as a miracle cure. But 10 rigorous studies, involving over 1,200 people, found zero benefit. The Canadian Institute for Health Research shut it down in 2022. Don’t waste time or money on it.
Same with extreme diets. No evidence that keto, paleo, or vegan diets reverse MS. Some people feel better eating clean-but that’s likely because they’re sleeping better, moving more, and reducing stress. Not because food magically heals myelin.
Living With MS: Real Life, Real Hope
Life expectancy for most people with MS is nearly normal. The biggest threats? Complications from immobility, like infections or blood clots-not the disease itself. With good care, many live full, active lives.
People with MS still work, raise kids, travel, and pursue passions. The key? Early treatment. Regular check-ins. Listening to your body. And finding support-whether it’s a local MS society, an online community, or a therapist who understands chronic illness.
MS isn’t a death sentence. It’s a challenge. And like any challenge, it’s easier to face with the right tools, the right team, and the right mindset.
Can you get MS if you’re over 50?
Yes, but it’s rare. Most people are diagnosed between 20 and 40. Late-onset MS (after 50) usually presents as primary progressive MS, with slower, steady decline. Symptoms can be mistaken for normal aging, so diagnosis often takes longer.
Is MS hereditary?
Not directly. You don’t inherit MS like eye color. But you can inherit genes that raise your risk. If a parent has MS, your chance is about 2-5%, compared to 0.1% in the general population. That’s higher than average, but still low.
Can stress make MS worse?
Stress doesn’t cause MS, but it can trigger relapses. Studies show people who report high stress levels are more likely to have flare-ups in the following weeks. Managing stress through mindfulness, therapy, or exercise isn’t optional-it’s part of treatment.
Do all people with MS need a wheelchair?
No. In fact, most don’t. About 75% of people with MS remain able to walk without assistance 15 years after diagnosis. Advances in treatment have made severe disability much less common than in past decades.
Can women with MS have children?
Yes. Pregnancy doesn’t make MS worse long-term. In fact, many women see fewer relapses during pregnancy, especially in the third trimester. The risk of relapse increases slightly in the first 3-6 months after birth, but overall, most women with MS have healthy pregnancies and babies. Talk to your neurologist about stopping or switching medications before conceiving.
Are there any natural cures for MS?
No. No supplement, diet, or alternative therapy has been proven to stop or reverse MS. Some people report feeling better with vitamin D, omega-3s, or acupuncture-but these help with symptoms, not the disease itself. Relying on unproven treatments instead of FDA-approved drugs can lead to irreversible damage.
Next Steps: What to Do If You Suspect MS
If you’re experiencing unexplained symptoms-vision loss, numbness, weakness, balance issues, or extreme fatigue that doesn’t go away-see a neurologist. Don’t wait. Early diagnosis means early treatment, and early treatment means better outcomes. Keep a symptom journal. Note when things happen, how long they last, and what makes them better or worse. Bring it to your appointment. You’re not just a patient-you’re the expert on your own body.
 Dec, 4 2025
Dec, 4 2025
aditya dixit
December 5, 2025 AT 19:08MS is one of those conditions where the body turns on itself like a corrupted program. What’s wild is how much environment plays a role-vitamin D, Epstein-Barr, even where you grew up. It’s not just genetics. It’s like your immune system got lost in the woods and started attacking trees thinking they’re bears.
Early treatment changes everything. I’ve seen people diagnosed in their 20s stay active into their 60s now. That’s not luck-it’s science catching up.
Mark Curry
December 6, 2025 AT 13:38It’s funny how we treat MS like it’s some monster. It’s just biology gone sideways. We fix broken pipes, we patch software… why do we freak out when the body does the same?
People say ‘you’re not defined by your illness’ but that’s easy to say when you’re not the one losing words mid-sentence. I just wish we treated it like hypertension-manageable, not tragic.
Ada Maklagina
December 7, 2025 AT 18:14fatigue is the real enemy not the wheelchair
Mellissa Landrum
December 8, 2025 AT 08:24they dont want you to know the real cause its all about the vaccines and the 5g towers and the glyphosate in your coffee theyre hiding the cure so pharma can keep selling those 80k a year drugs
Harry Nguyen
December 9, 2025 AT 14:24Of course the government pays for DMTs in the UK but here in America you’re expected to work two jobs just to afford a shot that doesn’t even cure you. Typical. We treat chronic illness like a personal failure, not a public health crisis.
Jennifer Patrician
December 10, 2025 AT 03:25Epstein-Barr? That’s just the tip. The real trigger is the mRNA vaccines they slipped into flu shots in 2021. Look at the spike in MS cases right after rollout. Coincidence? No. It’s the same people who told us smoking was safe. Wake up.
And don’t get me started on the WHO pushing vitamin D as a ‘risk factor’-they’re covering for the pharmaceutical lobby. My cousin’s neurologist got fired for saying the same thing.
Kylee Gregory
December 11, 2025 AT 13:52I think the most important thing people miss is that MS isn’t just a neurological condition-it’s a social one. The isolation from brain fog, the stigma around needing help, the way people assume you’re lazy if you’re tired… that’s the real damage sometimes.
Maybe the cure isn’t just in drugs but in how we treat each other.
Chris Brown
December 13, 2025 AT 13:15It is deeply troubling that society has normalized the idea that individuals with chronic illness must ‘adapt’ to a system designed for the able-bodied. The burden of accommodation should not rest upon the afflicted. Institutions must be restructured-not the patients.
Furthermore, the glorification of ‘early treatment’ as a moral imperative ignores the economic coercion embedded in healthcare systems. One cannot ‘choose’ therapy when one’s employer mandates 60-hour workweeks.
Philip Kristy Wijaya
December 14, 2025 AT 13:00Let me be the first to say this: the entire MS narrative is a manufactured crisis designed to sell drugs and justify neurologist salaries. You know what happens when you stop taking all those expensive DMTs? Most people live perfectly normal lives. The real problem is that we’ve turned a manageable condition into a life sentence because the medical-industrial complex needs revenue streams. The fatigue? Probably sleep apnea. The brain fog? Probably screen overload. The lesions? Could be migraines. We’ve pathologized normal human variation and called it a disease to sell pills. And now we’re all afraid to question it because the fear has been so well marketed.
My uncle had ‘MS’ for 30 years. Never used a wheelchair. Never took a single DMT. Died at 82 of heart disease. Funny how that never gets mentioned in the brochures.
And yes I know I’m the contrarian. But someone has to say it. The emperor’s not just naked-he’s wearing a lab coat and charging $87,000 a year for the privilege.