If you’ve seen small, round, pearly bumps on your child’s skin-or even your own-and wondered what they are, you’re not alone. Molluscum contagiosum is one of the most common viral skin infections in kids, but it shows up in adults too, especially after close contact or sexual activity. These bumps aren’t dangerous, but they’re contagious, annoying, and sometimes embarrassing. The good news? They usually go away on their own. The tricky part? Knowing when to wait and when to act.
What Molluscum Contagiosum Actually Looks Like
The telltale sign of molluscum contagiosum is a cluster of small, dome-shaped bumps. They’re usually 2 to 6 millimeters across-about the size of a pencil eraser. Their most distinctive feature? A tiny dimple or dot right in the center. That’s called an umbilication, and it’s a dead giveaway for doctors. The bumps can be white, pink, or match your skin tone. They don’t hurt, but they might itch, especially if you have eczema. They show up most often on the face, neck, arms, legs, and groin. In kids, they’re usually found on the arms, legs, or around the armpits. In adults, especially those who caught it through sexual contact, they cluster in the genital area or inner thighs. Unlike warts, which are rough and hard, molluscum bumps are smooth and soft. And unlike chickenpox blisters, they don’t burst and ooze. You won’t find them on the palms or soles of the feet.How It Spreads-and Why It Keeps Coming Back
The virus that causes molluscum is called MCV, short for molluscum contagiosum virus. It’s part of the poxvirus family, the same group that includes smallpox (but don’t worry-it’s nothing like that). You catch it through direct skin contact. That means hugs, wrestling, sharing towels, or even touching a doorknob someone with molluscum just touched. Swimming pools and shared gym equipment are common spread spots, especially for kids. It’s not airborne. You can’t catch it just by being in the same room. But once it’s on your skin, it can spread to other parts of your body if you scratch or pick at the bumps. Studies show scratching can triple the number of lesions in just a few weeks. Kids with eczema are at higher risk-about 30% more likely to get molluscum than kids with healthy skin. The virus thrives in warm, moist environments, which is why cases spike in summer and in tropical areas. The incubation period is 2 to 6 weeks. That means you could touch something infected and not see a bump for over a month. By then, you’ve already passed it on to others. That’s why it feels like it’s everywhere at once-it’s not one outbreak. It’s multiple silent infections that finally show up.Why Most Doctors Say: Just Wait
Here’s the thing most people don’t expect: the American Academy of Dermatology says the best treatment for most kids is no treatment at all. Why? Because molluscum clears up on its own in 6 to 24 months for 92% of healthy people. In fact, a long-term study from UC San Francisco found nearly all cases resolved without scarring by 18 months. Aggressive treatments like freezing (cryotherapy), scraping (curettage), or laser therapy can hurt, cause scarring, and sometimes make the infection worse by spreading the virus during the procedure. One survey of 1,204 patient reviews found that 41% of people felt their dermatologist recommended unnecessary treatments that left marks. For children, especially those with bumps on their face or arms, waiting is usually the safest and least stressful choice. Parents often report relief when they realize their child isn’t in danger and doesn’t need painful procedures. The CDC updated its guidelines in January 2023 to say: “No child should be excluded from school or swimming because of molluscum.” That’s a big shift from just a few years ago.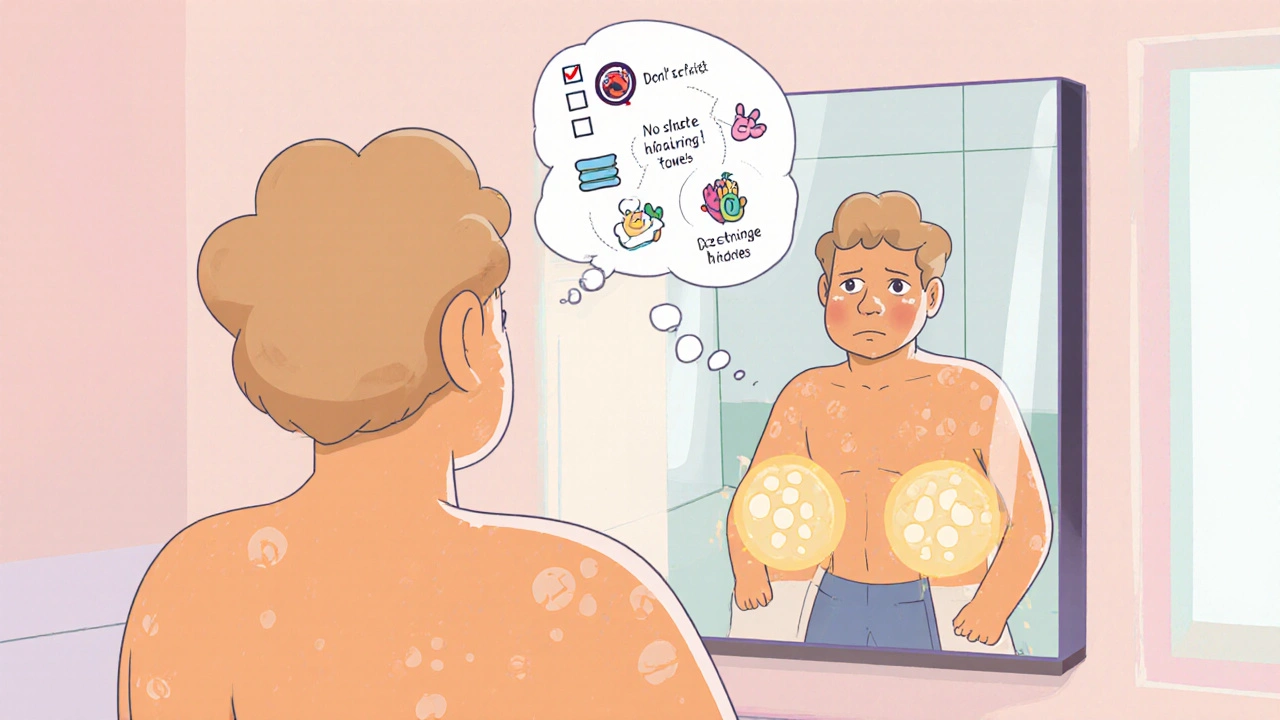
When You Should Treat It
Waiting works for most-but not everyone. Here’s when you should consider treatment:- Lesions on the genitals or face-especially in teens or adults. These can cause anxiety, affect relationships, or lead to teasing in school.
- More than 20 bumps-if the spread is rapid or overwhelming, treatment can help stop it.
- Signs of infection-redness, pus, swelling, or pain around a bump means bacteria got in. That needs antibiotics.
- Immunocompromised individuals-people with HIV, organ transplants, or cancer treatments can develop giant, persistent lesions (up to 3 cm) that don’t go away. These require medical intervention.
What Actually Works-And What Doesn’t
The Cochrane Review, which analyzes dozens of clinical trials, looked at 27 different treatments. The most effective? Cantharidin-a blistering agent applied by a doctor. It causes a small blister to form under the bump, lifting the virus out. Studies show it clears 73% of cases in 12 weeks, compared to 26% with a placebo. Other options include:- Topical potassium hydroxide (5-10%)-available in over-the-counter creams like MolluDab. Reviews show 63% of users cleared their bumps in 8 weeks with daily use.
- Imiquimod cream-a prescription immune booster. Works slowly but has fewer side effects than freezing.
- Cryotherapy-liquid nitrogen. Effective but painful. Risk of scarring, especially on delicate skin.
- Laser therapy-used for stubborn cases. Expensive and not usually covered by insurance.
How to Stop It from Spreading
If you or your child has molluscum, you can reduce transmission by doing just a few things:- Don’t scratch or pick. Cover bumps with a bandage if your child can’t resist.
- Don’t share towels, clothing, or bath sponges. CDC studies show this cuts household spread by 57%.
- Wash hands often. Especially after touching the bumps.
- Shower instead of bathe. Bath water can spread the virus to other parts of the body.
- Cover lesions during swimming. Many pools require this, even though the CDC says it’s not necessary for transmission.

What Adults Should Know
Adults with molluscum often get it through sexual contact. If you have bumps in your genital area, it’s important to get checked. While molluscum itself isn’t an STI like herpes or HPV, its presence can signal recent skin-to-skin contact with an infected partner. Avoid sexual activity until lesions are gone or fully covered. Many adults report emotional stress-especially around dating. One Reddit user shared how he avoided intimacy for 14 months until the bumps cleared. If you’re feeling anxious, you’re not alone. Treatment can help restore confidence. Topical potassium hydroxide or cantharidin are good first steps. Avoid freezing the genital area-it’s too painful and risky.What’s Next? New Treatments on the Horizon
Science is moving fast. In 2023, a new topical immunomodulator showed 82% clearance in a phase 2 trial-nearly double the rate of older treatments. It’s not available yet, but it’s a sign that better, gentler options are coming. Meanwhile, the CDC and WHO are watching how climate change might affect spread. Warmer, wetter climates could expand the virus’s range. But better hygiene and public awareness are helping balance that out.Bottom Line
Molluscum contagiosum is a nuisance, not a crisis. It’s common, contagious, and usually harmless. Most cases resolve without treatment. Aggressive interventions often cause more harm than good, especially in kids. The real goal isn’t to erase every bump-it’s to stop it from spreading and to protect your peace of mind. If you’re unsure, see a dermatologist. They can confirm it’s molluscum and help you decide whether to wait or treat. And remember: you’re not alone. Millions of families go through this every year. With patience and smart habits, it passes.Is molluscum contagiosum dangerous?
No, molluscum contagiosum is not dangerous. It’s a benign viral infection that doesn’t cause cancer or long-term health problems. In healthy people, it clears on its own without scarring. The only risks are secondary infections from scratching or emotional distress from visible bumps.
Can adults get molluscum contagiosum?
Yes. While it’s most common in children, adults can get it too-usually through sexual contact or close skin contact. Adults with weakened immune systems, like those with HIV, are at higher risk for severe, widespread outbreaks.
How long does molluscum last?
In healthy people, molluscum usually clears in 6 to 24 months. Most cases resolve by 18 months. In some people, especially those with eczema or weakened immunity, it can last up to 4 years. Treatment can speed things up, but it’s not always necessary.
Should I keep my child out of school or swimming?
No. The CDC and major health organizations no longer recommend keeping children out of school or swimming because of molluscum. The virus spreads through direct skin contact, not water or air. Covering bumps and practicing good hygiene is enough. Exclusion policies are outdated and cause unnecessary stress.
What’s the best over-the-counter treatment?
The most effective OTC option is a topical solution with 5-10% potassium hydroxide, like MolluDab. Clinical reviews show about 63% of users clear their bumps in 8 weeks with daily use. Avoid unproven remedies like tea tree oil or apple cider vinegar-they lack evidence and can irritate skin.
Can molluscum come back after it’s gone?
Once the infection clears, your body builds immunity, so you won’t get the same strain again. But you can get reinfected if you’re exposed to someone else with molluscum. It’s not a lifelong virus, but it’s not one-time immunity either.
Do I need to see a doctor?
You don’t always need to, but it’s smart to get a professional diagnosis. Other skin conditions like warts, eczema, or even skin cancer can look similar. A dermatologist can confirm it’s molluscum and advise on whether treatment is needed based on your age, health, and location of the bumps.
 Nov, 18 2025
Nov, 18 2025

Ellen Calnan
November 19, 2025 AT 02:06Okay but imagine being a kid with these bumps and just trying to live your life. I remember my cousin had them for two years-no one told us they’d just go away. We were terrified they were contagious in school, so she got isolated. Turns out? She was fine. The real villain here isn’t the virus-it’s the panic. We treat every little skin thing like a plague. We need to chill. The body knows what it’s doing. Let it heal. 🌱
Sam Reicks
November 20, 2025 AT 09:26they say wait but what if the doc is just lazy and dont wanna deal with it. i mean cmon. they got a whole $200 bill to charge you for freezing. why not do it? the virus is still there even if you cant see it. theyre hiding it. the pharma co is in bed with the aad. they want you to suffer so you buy more cream later. i saw a vid where a guy used duct tape for 3 weeks and it vanished. why is that not in the study? they dont want you to know
Chuck Coffer
November 20, 2025 AT 22:43Of course the dermatologists recommend waiting. They’re not paid by the hour. They’re paid by the procedure. Cryotherapy? $150. Cantharidin? $200. Wait-and-see? Free. You think they’re looking out for you? They’re looking out for their bottom line. And you’re the product.
Frank Dahlmeyer
November 21, 2025 AT 09:05Let me tell you something about molluscum-I’ve seen it firsthand in my nephew. He had 17 bumps on his arm, all perfectly round with that little dimple. We did nothing. No creams, no freezing, no panic. Just kept his nails short, washed his hands, and covered them with a Band-Aid at night. Six months later? Gone. Not a trace. And you know what? He didn’t miss a day of soccer. The real tragedy isn’t the bumps-it’s the overmedicalization of childhood. We’ve turned every minor skin issue into a crisis. We’ve forgotten how to trust the body. The immune system is not a broken machine. It’s a living, breathing warrior. Let it fight. Stop throwing chemicals at it. Let nature do its job. And if you’re an adult with it in your groin? Yeah, get it checked. But don’t let fear turn you into a walking anxiety attack. You’re not contagious to the whole world. Just to the people you hug too hard.
Paige Lund
November 21, 2025 AT 09:43So... just wait? Wow. Groundbreaking. I bet the CDC wrote this whole article after a coffee break.
Reema Al-Zaheri
November 21, 2025 AT 23:31It is important to note that molluscum contagiosum is caused by a double-stranded DNA virus belonging to the Poxviridae family, specifically molluscum contagiosum virus (MCV-1 to MCV-5). The incubation period ranges from two to six weeks, as stated, but transmission can occur via fomites, including towels, toys, and pool equipment, even without direct skin contact. Furthermore, the presence of atopic dermatitis significantly increases susceptibility, as the skin barrier is compromised. The efficacy of potassium hydroxide is supported by randomized controlled trials, with clearance rates of approximately 63% at eight weeks, as referenced. However, the use of cantharidin remains the most effective clinical intervention, with a 73% success rate. Home remedies such as apple cider vinegar lack any peer-reviewed evidence and may induce chemical burns. Therefore, while observation is often appropriate, it is not universally sufficient.
Michael Salmon
November 23, 2025 AT 15:33Wait? You’re telling me we’re supposed to just let a virus spread across a child’s body for two years? That’s not patience-that’s negligence. Parents are supposed to protect their kids, not hand them a pamphlet and say ‘good luck.’ And don’t even get me started on the ‘don’t scratch’ advice. Kids scratch. That’s what they do. You think a 4-year-old is gonna listen to a CDC brochure? This isn’t science. This is surrender dressed up as medical wisdom. Someone needs to step up and say: ‘We have tools. Use them.’
Joe Durham
November 24, 2025 AT 16:50I get where everyone’s coming from. I’ve been there-my daughter had molluscum on her neck, and I panicked. I Googled until 3 a.m. I was ready to book a cryo appointment. But then I talked to a nurse at the school clinic. She said, ‘Let’s wait a month. Watch how she’s doing.’ We did. She didn’t scratch. We kept her skin moisturized. And in six weeks? Half were gone. Now, at nine months, all of them are gone. No scars. No trauma. Just quiet healing. I think the real message here isn’t ‘wait’-it’s ‘trust.’ Trust your kid’s body. Trust the science. And trust that you don’t have to fix everything right now.
Derron Vanderpoel
November 25, 2025 AT 13:41i just want to say thank you for this post. my son had this and i felt so alone. everyone was like ‘oh it’ll go away’ but no one told me how to handle the guilt. like i was failing him by not rushing to the doctor. i cried reading this. we did nothing. just kept his hands clean and covered the bumps at night. he’s 10 now and it’s all gone. no scars. no drama. just a kid who got a weird rash and lived. you’re right-it’s not a crisis. it’s just life. 🙏
Timothy Reed
November 25, 2025 AT 14:52Thank you for this comprehensive and balanced overview. The emphasis on evidence-based outcomes, rather than fear-driven interventions, is both refreshing and necessary. The CDC’s updated guidelines reflect a mature understanding of the disease’s natural history. For parents and clinicians alike, the key is distinguishing between medical necessity and psychological discomfort. Treatment should be guided by clinical indicators-not parental anxiety. I’ve seen too many children subjected to painful procedures for lesions that would have resolved spontaneously. This post is a valuable resource for informed decision-making.
Christopher K
November 26, 2025 AT 19:05Wait for 2 years? That’s the American way-do nothing until it’s too late. In Germany, they freeze it on day one. In Japan, they use laser. We’re sitting here like peasants waiting for the virus to ‘heal itself.’ What’s next? Letting measles run its course? This isn’t science. It’s surrender. And it’s embarrassing.
harenee hanapi
November 28, 2025 AT 02:28My cousin’s daughter had it for three years and now she has scars on her face. Do you think that’s okay? No one told her parents to treat it. Now she won’t take pictures. She’s 16 and still avoids mirrors. And you’re telling me to wait? What if it’s your child? What if it’s your face? This isn’t just about ‘trust.’ It’s about responsibility. And you’re being irresponsible. I’m not mad. I’m just… heartbroken for families who didn’t know.
Christopher Robinson
November 29, 2025 AT 22:17✅ No school exclusion? ✅ No need to panic? ✅ Potassium hydroxide works? ✅ Duct tape doesn’t? 🙌 This is the kind of info we need more of. So many people are scared because they don’t know what’s real. This post cuts through the noise. Thanks for being clear, calm, and science-backed. I’m sharing this with every parent I know. 🌟
Angela Gutschwager
December 1, 2025 AT 10:57Just wait. 😌