For millions of women, menopause isn’t just about hot flashes and sleepless nights-it’s a turning point that affects bones, heart health, mood, and quality of life. Hormone therapy, often called HRT or menopause hormone therapy (MHT), has been around since the 1940s, but today’s understanding of it is nothing like what doctors believed in the 1990s. Back then, it was widely prescribed as a fountain of youth. Now, after decades of research, we know it’s not for everyone-but for many, it’s still the most effective tool available.
What Hormone Therapy Actually Does
Menopause hormone therapy replaces the estrogen (and sometimes progesterone) your body stops making after your last period. It doesn’t reverse aging. It doesn’t make you look younger. But it does something very specific: it shuts down the worst of menopause symptoms.
If you’re having 15 to 20 hot flashes a day, night sweats that soak your sheets, or brain fog so bad you forget where you put your keys, HRT can cut those symptoms by 75% or more. That’s not a small improvement-it’s life-changing. A 2021 study in JAMA Internal Medicine found that SSRIs and other non-hormonal drugs help, but only about half as much as estrogen therapy. Gabapentin? It reduces hot flashes by 45%, but leaves you dizzy. Herbal remedies like black cohosh? A 2020 Cochrane Review showed they barely beat placebo.
The real power of HRT isn’t just symptom relief. It also protects your bones. Estrogen slows bone loss. Women who skip HRT are far more likely to develop osteoporosis and break a hip after 60. One woman on a menopause forum wrote: “My DEXA scan stayed stable after 8 years on HRT. My sister, who refused it, broke her hip at 62.” That’s not anecdotal-it’s backed by decades of data.
The Risks Aren’t What You Think
When the Women’s Health Initiative study came out in 2002, it sent shockwaves through medicine. It linked HRT to higher risks of breast cancer, heart attacks, and strokes. Millions of women stopped taking it overnight. But here’s what the headlines didn’t tell you: the study mostly included women over 60, many of whom had been through menopause for over a decade. That’s the problem.
Today, doctors call this the “timing hypothesis.” Starting hormone therapy within 10 years of your last period-or before age 60-makes a huge difference. For women in that window, the benefits often outweigh the risks. For those starting later, the risks climb.
Let’s break down the numbers:
- Estrogen-only therapy (for women without a uterus) adds about 9 extra breast cancer cases per 10,000 women per year. That’s small.
- Estrogen plus progestogen adds about 29 extra cases per 10,000 women per year. Still low, but higher.
- Oral estrogen increases the risk of blood clots by about 3 per 1,000 women per year. Transdermal (patch or gel) cuts that risk in half.
- Oral estrogen raises stroke risk by 30% compared to transdermal, according to the E3N study of 76,000 women.
These aren’t trivial numbers-but they’re not terrifying either. For a 52-year-old woman with severe hot flashes, the risk of a stroke or clot might be 0.3% per year. For a 70-year-old woman with no symptoms, that same risk isn’t worth it.
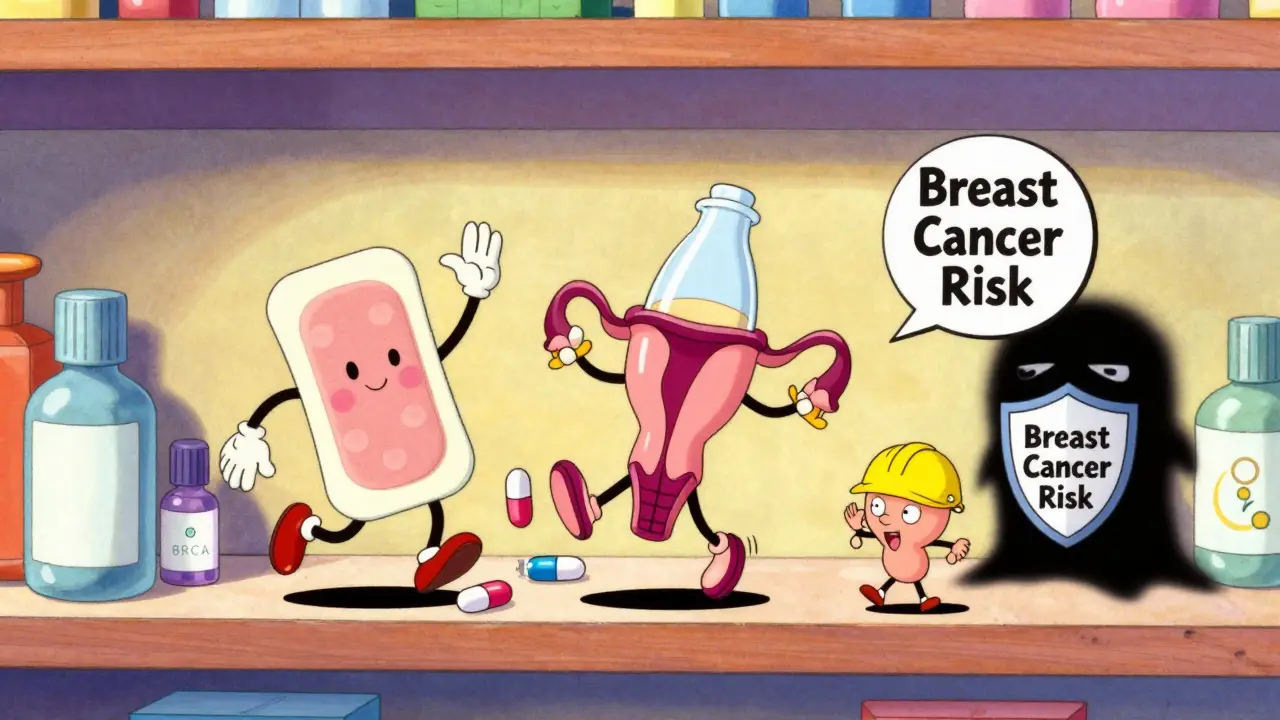
Which Type of HRT Is Right for You?
Not all hormone therapy is the same. The delivery method and hormone type change everything.
Oral estrogen (like Premarin or generic estradiol pills) goes through your liver first. That’s why it raises clot and stroke risk more. It’s cheaper-$15 to $30 a month for generics-but not always the safest.
Transdermal estrogen (patches, gels, sprays) enters your bloodstream directly. It avoids the liver. That means lower clot risk, lower stroke risk, and fewer side effects like bloating. Doses range from 0.025 mg to 0.1 mg per day. Many women start with 0.05 mg.
Progestogen is only needed if you still have a uterus. Without it, estrogen can cause endometrial cancer. Micronized progesterone (like Prometrium) is preferred over older synthetic versions like medroxyprogesterone acetate (Provera). It’s gentler on mood and has less impact on breast cancer risk.
Vaginal estrogen (creams, rings, tablets) treats dryness and discomfort during sex but doesn’t help hot flashes. It’s safe for long-term use and doesn’t affect the rest of your body much.
There’s also a newer option: Duavee. It combines estrogen with bazedoxifene, a drug that protects the uterus without needing extra progesterone. It’s pricier-$300 to $400 a month-but good for women who can’t tolerate progesterone.
Who Should Avoid HRT?
HRT isn’t for everyone. You should not start it if you have:
- A history of breast cancer
- Active blood clots or deep vein thrombosis
- Pulmonary embolism
- Uncontrolled high blood pressure
- History of stroke or heart attack
- Severe liver disease
- Unexplained vaginal bleeding
Family history of breast cancer? That doesn’t automatically rule you out-but it does mean you need to be extra careful. Talk to your doctor about your personal risk, not just your mother’s or sister’s history.

What to Expect When You Start
Most women notice improvement in hot flashes within 10 days to 4 weeks. Some feel better in just a few days. But side effects can show up too.
Breakthrough bleeding is common in the first 3 to 6 months. It’s usually harmless and fades with time. If it keeps happening after 6 months, your dose may need adjusting.
Mood swings, breast tenderness, and bloating are also common at first. These often settle down. If they don’t, switching from oral to transdermal estrogen or changing the type of progesterone can help.
One woman on Reddit wrote: “I went from 15-20 hot flashes daily to 2-3 within 10 days on 0.05 mg estradiol patch.” That’s not rare. A 2024 survey of over 1,200 women found 68% had “dramatic improvement.”
But 22% didn’t feel better. Why? Maybe the dose was too low. Maybe they needed progesterone. Or maybe their symptoms weren’t hormonal at all. Depression, thyroid issues, and sleep apnea can mimic menopause symptoms. That’s why a full check-up is essential before starting.
How Long Should You Stay on It?
There’s no one-size-fits-all answer. Most women take HRT for 3 to 5 years. Some stay on longer-for bone protection, for quality of life, because they feel better.
Experts agree: use the lowest dose that works, for the shortest time needed. But if you’re still having severe symptoms at 60, and you’re otherwise healthy, there’s no rule saying you have to quit.
The 2022 Endocrine Society guidelines say: if you started before 60 and are doing well, continuing past 5 years is reasonable. The goal isn’t to stop at 5 years-it’s to avoid staying on longer than you need to.
Many women stop because they’re scared of breast cancer. A 2023 survey found 72% quit due to fear, not side effects. But fear isn’t always based on facts. For many, the risk is lower than they think.
Alternatives to Hormone Therapy
If HRT isn’t right for you, there are other options-but none are as effective.
- SSRIs (like escitalopram or paroxetine): Reduce hot flashes by 50-60%. Useful if you also have anxiety or depression.
- Gabapentin: Reduces hot flashes by 45%. Causes dizziness in 1 in 4 users.
- Clonidine: A blood pressure drug that helps some women. Causes dry mouth and drowsiness.
- Phytoestrogens (soy, flaxseed, red clover): Cochrane Review found they reduce hot flashes by less than half a day per week-barely better than placebo.
- Cognitive behavioral therapy (CBT): Helps with sleep, mood, and coping. Doesn’t stop hot flashes but makes them easier to handle.
None of these match HRT’s effectiveness. But they’re worth trying if you can’t or won’t take hormones.
What’s Changing in 2026?
The conversation around HRT is shifting fast. In July 2025, the FDA opened a public docket asking for more data on how age, timing, and delivery method affect risk. A landmark study presented at The Menopause Society’s 2025 Annual Meeting analyzed 120 million patient records and found that starting estrogen during perimenopause-before your last period-cut cardiovascular risk by 18% compared to starting after menopause.
That’s huge. It means the clock starts ticking before your period ends. If you’re in your late 40s and having irregular cycles, now might be the best time to talk to your doctor.
Doctors are also moving toward personalized care. Within five years, genetic tests may tell you how your body metabolizes estrogen-helping choose the right dose and type. Some clinics already offer this.
Meanwhile, big employers are stepping in. 42% of Fortune 500 companies now offer menopause support programs. That’s not just perks-it’s recognition that this isn’t a minor inconvenience. It’s a health issue that affects work, focus, and well-being.
Where to Start
If you’re considering HRT, here’s how to begin:
- Track your symptoms for a month. Use a journal or app. Note frequency of hot flashes, sleep issues, mood changes.
- See your doctor. Ask for blood pressure check, thyroid test, and bone density scan if you’re over 55.
- Discuss your personal and family history. Be honest about any past clots, cancer, or heart issues.
- Ask: “Am I under 60 or within 10 years of menopause?” If yes, HRT is likely safe for symptom relief.
- Start with the lowest dose of transdermal estrogen. Add micronized progesterone only if you have a uterus.
- Re-evaluate in 3 months. Do symptoms improve? Are side effects manageable?
Don’t be pressured to quit after 5 years if you still need it. Don’t be scared off by old headlines. The data now is clearer than ever: for the right woman, at the right time, HRT works.
Final Thoughts
Menopause doesn’t have to be a battle you fight alone. Hormone therapy isn’t a magic cure. But for women with moderate to severe symptoms, it’s the most powerful tool we have. The risks are real-but they’re not universal. They depend on your age, your health, your family history, and how you take it.
Don’t let fear silence your questions. Talk to a provider who knows the latest guidelines-not the ones from 2003. Use the North American Menopause Society’s directory to find a certified menopause practitioner. You deserve relief. You deserve to feel like yourself again.
Is hormone therapy safe for women under 60?
Yes, for most healthy women under 60 or within 10 years of menopause onset, hormone therapy is considered safe and effective for managing symptoms. Major medical groups like NAMS and the Endocrine Society agree that benefits outweigh risks in this group, especially when using the lowest effective dose and transdermal delivery methods.
Does HRT cause breast cancer?
Estrogen plus progestogen therapy slightly increases breast cancer risk-about 29 extra cases per 10,000 women per year. Estrogen-only therapy (for women without a uterus) shows no significant increase. Risk rises with longer use, but for most women taking it short-term for symptoms, the absolute risk remains low.
What’s the best way to take HRT: pill, patch, or gel?
Transdermal options (patches or gels) are generally safer than oral pills. They avoid liver metabolism, reducing the risk of blood clots and stroke by up to 50%. For women with a history of clotting issues or high blood pressure, transdermal is the preferred choice.
How long should I stay on hormone therapy?
There’s no fixed time limit. Most women take it for 3 to 5 years. But if symptoms persist after that and you’re otherwise healthy, continuing beyond 5 years is reasonable. The goal is to use the lowest dose for the shortest time needed-not to quit arbitrarily at 5 years.
Can I use HRT if I have a family history of breast cancer?
A family history doesn’t automatically rule out HRT, but it requires careful discussion with your doctor. Your personal risk profile matters more than your relatives’ history. If you’re a carrier of BRCA mutations, alternatives may be preferred. For others, low-dose transdermal estrogen may still be an option with close monitoring.
Do I need progesterone if I’ve had a hysterectomy?
No. If you’ve had a hysterectomy, you don’t need progesterone. Estrogen alone is safe and effective. Adding progesterone when it’s not needed increases side effects and breast cancer risk without benefit.
What are the side effects of HRT?
Common side effects include breast tenderness, bloating, mood swings, and breakthrough bleeding-especially in the first few months. These often improve with time or by switching formulations. Serious side effects like blood clots or stroke are rare but more likely with oral therapy and in women over 60.
Can HRT help with weight gain during menopause?
HRT doesn’t directly cause weight loss, but it can help manage fat distribution. Estrogen helps prevent abdominal fat buildup, which is common after menopause. While it won’t melt pounds, it may help you maintain a healthier body shape and reduce metabolic risks.
Are natural or herbal options as good as HRT?
No. Herbal remedies like black cohosh, soy, or red clover show minimal benefit in clinical trials. A Cochrane Review found they reduce hot flashes by less than half a day per week-barely better than a placebo. They’re not dangerous, but they’re not a substitute for proven hormone therapy when symptoms are severe.
When should I stop HRT?
There’s no set age to stop. If your symptoms are gone and you’re not using it for bone protection, you can try tapering off after 3-5 years. But if you still have hot flashes, night sweats, or bone loss, continuing is reasonable. Always discuss stopping with your doctor-it’s not a one-size-fits-all decision.
Menopause is a natural phase of life, but it doesn’t have to be a painful one. With the right information and care, you can navigate it with strength-and yes, with relief.
 Jan, 6 2026
Jan, 6 2026

Kyle King
January 7, 2026 AT 00:05Yeah right, HRT is just Big Pharma’s way of keeping women docile. They’ve been lying since the 50s. Ever wonder why every woman over 50 suddenly needs a prescription? It’s not medicine-it’s control. And don’t even get me started on those ‘transdermal patches’-they’re just fancy glitter patches with estrogen poison inside. The FDA’s been bought. Read the leaked emails.
Emma Addison Thomas
January 7, 2026 AT 14:05I’ve been on low-dose estradiol gel for three years now. My hot flashes dropped from 15 a day to maybe two. I didn’t feel like I was ‘taking hormones’-I felt like I got my brain back. The fear around HRT feels outdated. My GP checked my bone density and cholesterol-both improved. It’s not magic, but it’s not poison either.
Mina Murray
January 8, 2026 AT 14:03Let’s be real-this whole article is a slickly packaged ad for pharma. Black cohosh doesn’t work? Says who? The same journals that got paid by Wyeth back in 2002. And ‘transdermal is safer’? Tell that to the 3 women in my book club who got DVT after switching to patches. You think they told their doctors? Nah. They just stopped and suffered. Also, ‘micronized progesterone’ sounds fancy but it’s still synthetic. And why is no one talking about the fact that estrogen is a carcinogen? It’s in every plastic bottle. You’re just giving it to yourself now.
Rachel Steward
January 9, 2026 AT 05:28You’re all missing the forest for the trees. The real issue isn’t whether HRT works-it’s why we’ve allowed women’s bodies to be treated like broken machines that need a chemical fix. We’ve medicalized natural biology so hard that now women think they’re defective if they feel a hot flash. And yes, estrogen reduces symptoms-but it also suppresses the body’s own adaptive mechanisms. The real solution isn’t more hormones-it’s better sleep hygiene, less sugar, stress reduction, and community support. But that doesn’t sell pills. So we get 12-page articles with pretty graphs and zero existential depth. You want to feel like yourself again? Stop trying to chemically erase menopause. Start living through it.
Christine Joy Chicano
January 9, 2026 AT 22:47There’s something quietly revolutionary about how much the science has shifted since 2002. Back then, it was ‘HRT = breast cancer = avoid at all costs.’ Now we understand timing, delivery, and individual risk profiles. It’s not just about estrogen-it’s about *how* it’s delivered, *when* it’s started, and *who* you are. That’s precision medicine in action. And the fact that 42% of Fortune 500 companies now offer menopause support? That’s not corporate virtue signaling-it’s economic recognition that women’s health impacts productivity, retention, and innovation. This isn’t a women’s issue. It’s a societal one.
Adam Gainski
January 10, 2026 AT 15:39As a guy married to someone who went through this, I just want to say: thank you for writing this clearly. My wife was terrified of HRT after hearing the old WHI scare stories. We went to a certified menopause specialist, did the bloodwork, got the DEXA scan, and started her on a 0.05 mg patch. Within two weeks, she was sleeping through the night. She’s not ‘cured’-but she’s back. I wish more men understood this isn’t just ‘mood swings’-it’s a physiological overhaul. Support isn’t about fixing it. It’s about listening.
Anastasia Novak
January 10, 2026 AT 21:32Oh my god, another ‘HRT is safe if you’re under 60’ article. So what? I’m 58, had a hysterectomy at 40, and I’ve been on estrogen since 2015. I don’t care about your ‘low-dose’ or ‘transdermal’-I care that I don’t feel like I’m melting inside every afternoon. You talk about risks like they’re math problems. I’m not a statistic. I’m a woman who can’t sleep, can’t focus, and can’t even walk to the mailbox without sweating through three shirts. If taking a patch means I don’t have to cry in the shower every day, then yes-I’ll take the ‘slightly higher’ breast cancer risk. I’m not dying of hot flashes. I’m dying of boredom. And this? This is my rebellion.
Jonathan Larson
January 12, 2026 AT 15:29The evolution of medical understanding regarding hormone therapy exemplifies the scientific method in practice: hypothesis, data, revision, and refinement. The Women’s Health Initiative was a landmark study, yet its limitations-particularly regarding cohort age and hormonal formulation-were not adequately contextualized in public discourse. Contemporary guidelines reflect a nuanced, evidence-based recalibration. The imperative now is not fear, but informed autonomy. Women deserve access to accurate, individualized counsel-not sensationalized headlines or ideological dogma. This article fulfills that duty admirably.
Kamlesh Chauhan
January 14, 2026 AT 01:01why do they always make it sound like its a choice when its just your body falling apart and everyone telling you to take pills like its a coffee habit. i dont wanna be on hormones i just wanna not feel like i’m on fire all the time. who even made this rule that you have to be under 60 to not die from sweating
Alex Danner
January 15, 2026 AT 14:29Just had my 6-month check-in on the estradiol patch. Breakthrough bleeding stopped after month 4. My mood? Stable. My sleep? Actually sleeping. And yes, I’m still paranoid about breast cancer-but I’m also not dying of hot flashes at 5:30 a.m. My doctor said if I’m feeling good at 65, we’ll reassess. That’s the key: it’s not a yes/no decision. It’s a living plan. And if you’re scared? Talk to a menopause specialist, not your aunt who read a blog in 2005.
Katrina Morris
January 16, 2026 AT 06:30i just started the patch last month and honestly i thought it was gonna be this huge deal but its just… a patch? and now i can watch tv without sweating through my shirt? i dont know why everyone makes it sound so scary. i mean, i still eat ice cream and cry at commercials but now i can do it in comfort. also i spelled everything wrong here i think
steve rumsford
January 16, 2026 AT 18:32my wife took it for 2 years and now she says she feels like she’s 35 again. not literally but you know what i mean. i dont get the drama. if it helps you sleep and not melt in the grocery store, why are people acting like you’re injecting Satan?