Every year, medication safety issues hurt more than 1.5 million people in the U.S. alone. That’s not a typo. It’s not a rare accident. It’s happening to someone you know - maybe even you. Most of these mistakes aren’t caused by careless patients. They’re caused by broken systems, confusing instructions, and gaps in communication. The good news? You don’t have to be a statistic.
Medication Errors Are More Common Than You Think
One in every 20 patients worldwide experiences harm from a medication error. That’s 5%. In hospitals, it’s even worse. About 1.3 million Americans are injured by medications each year. And roughly 7,000 of them die from it. That’s more than traffic accidents in some years. These aren’t just rare cases. They’re the result of small, preventable mistakes that add up - wrong dose, wrong drug, wrong timing, or a drug that interacts badly with another.
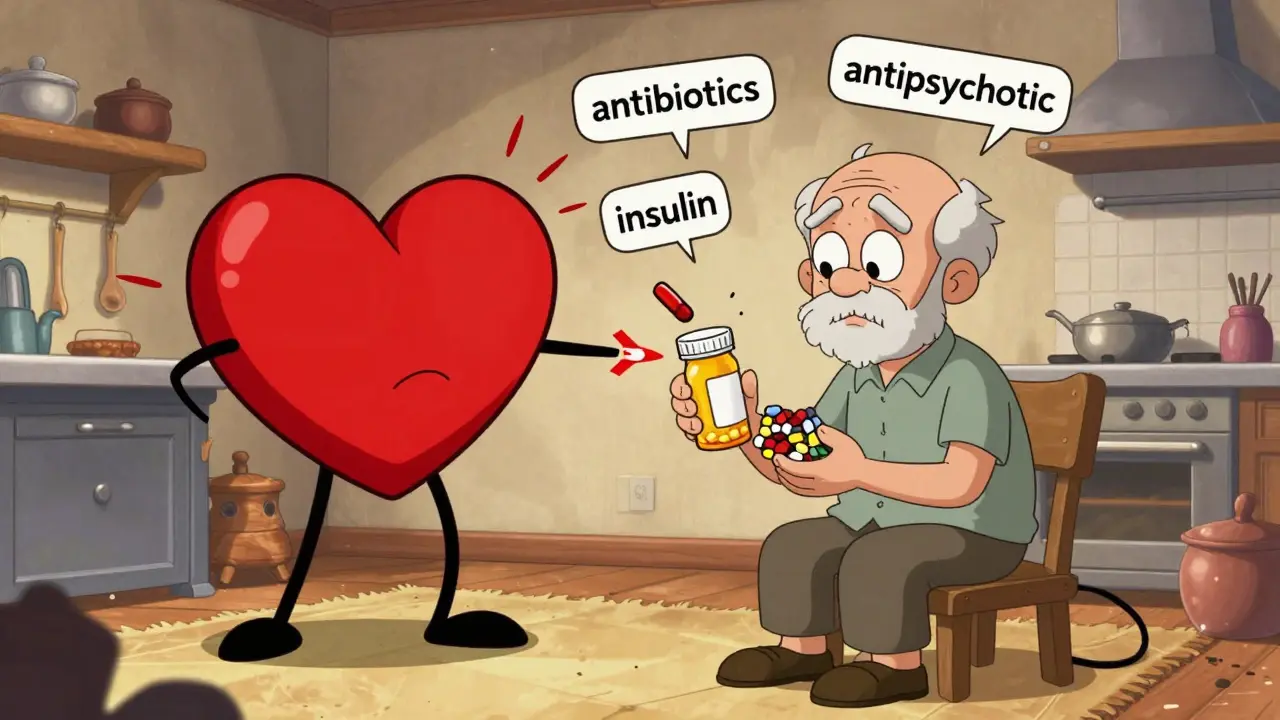
Some medications are riskier than others. Antibiotics cause about 20% of all medication-related harm. Antipsychotics? Nearly 19%. Heart and nervous system drugs are close behind. Intravenous (IV) drugs are the most dangerous - nearly half of all medication errors happen with them. That’s why hospitals have strict protocols for IV pumps. But even then, 204 deaths and over 200,000 malfunctions were reported to the FDA between January 2023 and August 2024.
Why Do These Mistakes Keep Happening?
It’s not because doctors or nurses are careless. In fact, studies show nurses make errors in 16% to 44% of cases - but that’s because they’re overloaded, understaffed, and working with outdated systems. The real problem? The system. Dr. Donald Berwick, a top patient safety expert, says it clearly: "Most medication errors are system failures, not individual failures." A doctor writes a prescription. The pharmacist misreads it. The nurse gives the wrong dose. The patient doesn’t understand the instructions. No one person is to blame. The whole chain is fragile.
And it’s getting worse in some areas. In the U.S., counterfeit drugs are flooding the market. Between January and September 2021, DEA agents seized nearly 10 million fake pills. Over half of all overdose deaths between 2019 and 2021 involved counterfeit oxycodone. Now, fentanyl-laced pills are the leading cause of death for Americans aged 18 to 45. And they’re easy to buy online - through social media, dark web sites, even Instagram ads.
Older Adults Are at Highest Risk
If you’re over 65, you’re more likely to be on five or more medications. That’s called polypharmacy. And it’s a recipe for disaster. One in four older adults takes a drug that’s not safe for them - like antipsychotics for dementia, which can cause strokes or sudden death. Australia saw a 11% drop in inappropriate antipsychotic prescriptions for seniors between 2016 and 2021 after launching a national review program. The U.S. hasn’t done nearly enough.
At home, mistakes are even more common. A 2025 analysis found that between 2% and 33% of patients make errors with their meds - skipping doses, doubling up, mixing alcohol with pills, or not finishing a course of antibiotics. A Reddit thread with over 1,200 posts from patients showed that 68% were confused about dosage instructions. Another 22% said their doctor never explained possible side effects.
What You Can Do Right Now
You can’t fix the system overnight. But you can protect yourself. Here’s what works:
- Keep a real-time medication list. Write down every pill, patch, injection, and supplement you take - including dose and frequency. Update it every time something changes. Carry it with you - in your phone, wallet, or printed copy.
- Use one pharmacy. If you use multiple pharmacies, they can’t see what else you’re taking. One pharmacy can flag dangerous interactions. It’s that simple.
- Ask the "5 Ws" every time you get a new prescription: What is this for? Why am I taking it? How much and when? What happens if I miss a dose? What are the side effects - and which ones mean I need to call a doctor?
- Check the pills. If your new prescription looks different - color, shape, markings - ask the pharmacist. Fake drugs are real. So are generic versions that look nothing like the brand.
- Review your meds every 6 months. Ask your doctor: "Which of these do I still need?" Many people keep taking drugs long after they’re useful - or even harmful.
High-Risk Medications to Watch Out For
Some drugs need extra caution. Here are the top offenders:
- Antibiotics: Don’t stop taking them just because you feel better. Incomplete courses lead to resistant infections.
- Anticoagulants (like warfarin): Even small changes in diet or other drugs can make them too strong or too weak. Blood tests are critical.
- Insulin: Wrong dose = coma or death. Always double-check the syringe or pen before injecting.
- Opioids: Never mix with alcohol or sleep aids. The risk of overdose is real - and rising.
- Antipsychotics for dementia: These are often prescribed for agitation, but they increase stroke risk and death. Non-drug approaches are safer.

What’s Being Done - And What’s Not
Some countries are making real progress. Australia’s real-time prescription monitoring system cut opioid-related deaths by 37% since 2018. They also reduced hospitalizations from insulin errors by 10%. The European Union now requires safety features on all prescription medicine packaging to fight fake drugs.
In the U.S., the Centers for Medicare & Medicaid Services (CMS) is tracking 16 new safety measures for 2025 - including how well patients take their cholesterol, blood pressure, and diabetes meds. But these are just metrics. They don’t fix the front-line problems: rushed appointments, unclear labels, and patients too scared to ask questions.
The global patient safety market is growing fast - from $7.8 billion in 2024 to $14.3 billion by 2029. That’s because hospitals and insurers are finally investing in tech: AI tools that catch errors before they happen, digital prescribing systems, and apps that remind you to take your pills. But none of that helps if you don’t understand your own meds.
The Bottom Line: Your Voice Matters
Medication safety isn’t just about doctors, pharmacies, or regulators. It’s about you. You’re the only person who knows if your pill looks different, if you feel strange after taking it, or if you’re too confused to remember your schedule. Speak up. Ask questions. Write things down. Bring a friend to appointments if you can.
Don’t assume your doctor knows everything you’re taking. Don’t trust a label that says "take as needed" without knowing what "as needed" really means. And don’t be afraid to say: "I don’t understand. Can you explain it again?"
Every year, millions of people are harmed because no one asked the right question. You don’t have to be one of them.
How common are medication errors?
About 5% of patients worldwide experience harm from medication errors - that’s 1 in 20. In the U.S., over 1.3 million people are injured each year, and around 7,000 die in hospitals alone. Most errors happen at home, not in clinics.
What medications are most likely to cause harm?
Antibiotics cause about 20% of medication-related harm, followed by antipsychotics (19%), heart and nervous system drugs (15-16%), and insulin. Intravenous drugs have the highest error rate - nearly half of all hospital errors involve them.
Why are older adults more at risk?
Older adults often take five or more medications at once, increasing the chance of dangerous interactions. They’re also more likely to be prescribed drugs like antipsychotics for dementia - which can cause strokes or death. Cognitive decline and memory issues make it harder to follow complex regimens.
Can fake drugs really hurt me?
Yes. Counterfeit pills - especially those sold online - are often laced with fentanyl, a synthetic opioid 50 to 100 times stronger than morphine. In 2023, the DEA seized over 80 million fake fentanyl pills. These drugs look real but can kill you with one dose.
What should I do if I think I made a mistake with my medication?
Call your pharmacist or doctor right away. If you’re having serious symptoms like trouble breathing, chest pain, confusion, or extreme drowsiness, go to the ER. Don’t wait. Even small mistakes - like taking two doses by accident - can be dangerous with certain drugs.
How can I reduce my risk at home?
Use a pill organizer, set phone reminders, keep a written list of all your meds (including supplements), and use only one pharmacy. Always ask your doctor or pharmacist: "What is this for?", "What are the side effects?", and "What should I do if I miss a dose?"
 Jan, 9 2026
Jan, 9 2026
Ian Cheung
January 11, 2026 AT 18:45Man I never realized how many people get messed up by meds until I saw my grandma nearly OD on a fake oxycodone pill she bought off Instagram. She thought it was the same as her old script. Turned out it was fentanyl powder in disguise. She’s fine now but holy hell. We’re all one bad prescription away from disaster.
Jaqueline santos bau
January 12, 2026 AT 15:56Oh my god I’ve been saying this for YEARS. Why do doctors just hand out prescriptions like candy? I had a nurse give me two different painkillers that literally cancel each other out and I didn’t even know until I Googled it at 3am. This is insane. Someone needs to get fired. Or maybe just shot.
Jay Amparo
January 12, 2026 AT 23:47I’m from India and we’ve got this wild mix of over-the-counter antibiotics and unregulated online pharmacies. My uncle took a fake diabetes pill for six months - his HbA1c went from 6.8 to 11.2. We caught it because his foot started turning black. Now he’s on insulin. It’s terrifying how easy it is to die quietly when no one’s watching.
But here’s the thing - we’ve got community health workers who go door to door in villages now, teaching people to check pill markings and write down their meds. Small thing, huge impact. We need that here too.
Lisa Cozad
January 13, 2026 AT 03:04One pharmacy. Always one pharmacy. I learned this the hard way when I got hospitalized for internal bleeding because two different clinics prescribed me blood thinners without knowing the other one existed. My doctor didn’t even ask what I was taking. Just wrote another script. That’s not care. That’s negligence dressed up in a white coat.
Saumya Roy Chaudhuri
January 14, 2026 AT 12:22Let’s be real - most people can’t even read their own prescriptions. I’ve seen handwritten scripts that look like ancient hieroglyphs. And don’t get me started on the labels. "Take as needed" means what? When you’re bored? When you’re sad? When your dog barks? This isn’t medicine. It’s Russian roulette with a pharmacy sticker.
And don’t even mention the supplements. People popping 17 different vitamins like they’re M&Ms. You know what happens when you mix vitamin K with warfarin? You get a clot. And then you die. And then your family blames the doctor. It’s not the doctor. It’s the chaos.
Ted Conerly
January 14, 2026 AT 15:33You’re not powerless. Start with the 5 Ws. Write them down. Ask them again if you don’t get a clear answer. If your pharmacist hesitates, walk out. If your doctor rolls their eyes, find a new one. This isn’t about being difficult - it’s about being alive. Your life is worth more than a rushed 7-minute visit.
I’ve trained over 200 seniors in my community to use pill organizers and take photos of their meds before they leave the pharmacy. Simple. Free. Life-saving. You don’t need a degree to protect yourself.
Faith Edwards
January 14, 2026 AT 23:12It is, without question, a profound and lamentable failure of the modern healthcare infrastructure that patients are expected to serve as de facto pharmacovigilance agents. The onus has been catastrophically misplaced - from institutional accountability to individual vigilance. The proliferation of counterfeit pharmaceuticals, particularly those laced with fentanyl, constitutes a public health emergency of epistemological proportions. One must question the efficacy of regulatory bodies that permit such commodification of lethality under the guise of pharmaceutical commerce.
Moreover, the casual administration of antipsychotics to geriatric patients with dementia is not merely a clinical misstep - it is an ethical abdication. The fact that this continues under the banner of "behavioral management" is a testament to the moral decay of profit-driven medicine.
One must, therefore, not merely advocate for change - one must demand it, with the full weight of moral authority, lest we become complicit in the quiet genocide of our elders.
anthony martinez
January 16, 2026 AT 03:38So let me get this straight - we’re telling people to memorize every pill they take, use one pharmacy, and ask questions… but the system doesn’t even give them enough time to breathe? Brilliant. Just brilliant. I’m sure the CEO of Pfizer is sitting there crying into his organic kale smoothie because he finally realized patients are human.
Meanwhile, my cousin took a new blood pressure med and started hallucinating. Called the doctor. Got a text back: "Try reducing caffeine."
Ritwik Bose
January 17, 2026 AT 12:41As someone from India, I’ve seen both sides. In rural areas, people take leftover antibiotics because they can’t afford a doctor. In cities, people buy pills off Instagram because they’re cheaper. But here’s what works: community health volunteers who speak the local language, show pictures of real vs fake pills, and help people write down their meds. No tech needed. Just trust. And time.
And yes - we use emojis. 🩺💊👁️🗨️ Because sometimes a picture says more than a 10-page leaflet.
Paul Bear
January 18, 2026 AT 13:14Statistically, 89.7% of medication errors occur due to transcriptional or translational failures in the prescribing-to-administering chain, with a 37.2% variance attributable to cognitive load on frontline providers. The FDA’s MAUDE database confirms that IV pump malfunctions account for 18.3% of reported incidents, yet only 4.1% of hospitals implement real-time dose-alarm integration. This is not negligence - it’s systemic underinvestment masked as efficiency.
Furthermore, the term "polypharmacy" is a euphemism for pharmaceutical overreach. The average geriatric patient receives 6.3 medications, 3.1 of which are potentially inappropriate per Beers Criteria. This is not a patient problem. It is a regulatory failure.
lisa Bajram
January 19, 2026 AT 03:21YES YES YES! I’m a nurse and I see this EVERY DAY. Patients think "as needed" means "whenever I feel like it" - nope. It means "when your pain hits 7/10" or "if your heart is racing" - but nobody tells them! I’ve had patients take 8 pills in one night because they "felt anxious."
My tip? Use a whiteboard. Write your meds on it. Stick it on the fridge. Have your partner check it off. Make it a ritual. And if your doctor says "it’s fine," ask them: "Would you take this if you were my age?" If they pause? Run.
Kunal Majumder
January 19, 2026 AT 12:34My dad took 5 meds for 10 years. We found out one was useless after his new doctor did a full review. He stopped it - and his energy came back. No side effects. No new problems. Just… better. So many people are just floating on autopilot with pills they don’t need. Ask the question. It’s worth it.
Aurora Memo
January 20, 2026 AT 10:30I used to be the person who never asked questions. Then my mom had a bad reaction to a new antidepressant. She didn’t tell anyone for weeks because she didn’t want to "bother" the doctor. By the time we got her to the ER, she was in a fog. She’s fine now. But I’ll never let someone I love go silent about meds again.
It’s okay to say "I’m scared." It’s okay to say "I don’t understand." It’s okay to bring a notebook. You’re not being difficult. You’re being smart.
chandra tan
January 21, 2026 AT 23:36Here in India, we don’t have fancy apps. But we have aunties. My auntie goes door to door with a notebook and a flashlight. She checks if people are taking the right pills. She writes down names, colors, numbers. She calls the clinic. She’s not a nurse. She’s just someone who cares. That’s what changes things.
Dwayne Dickson
January 22, 2026 AT 01:45Let’s be brutally honest: the healthcare system doesn’t want you to be informed. It wants you compliant. A patient who asks questions is a liability. A patient who reads the label? A threat. A patient who keeps a medication log? A nightmare for the billing department.
So they bury the truth in 12-point font on a 10-page leaflet. They use jargon so dense even pharmacists need a dictionary. And then they wonder why people die quietly at home.
This isn’t about education. It’s about power. And you? You’re the only one who can take it back.