Generic drugs make up 90% of prescriptions in the U.S. - but how do we know they’re as safe as brand-name ones?
If you’ve ever picked up a generic pill at the pharmacy, you’ve probably wondered: Is this really the same as the brand-name version? The answer isn’t just "yes" - it’s backed by one of the most rigorous drug oversight systems in the world. The FDA is the U.S. agency responsible for ensuring that every generic drug sold in America meets the same strict standards for safety, strength, quality, and performance as its brand-name counterpart. This isn’t guesswork. It’s a multi-layered system built on science, inspections, and continuous monitoring.
Here’s the key: Generic drugs don’t need to repeat the expensive clinical trials that brand-name drugs go through. Instead, they must prove they’re bioequivalent - meaning they deliver the same amount of active ingredient into the bloodstream at the same rate. The FDA requires this to be within 90-110% of the brand-name drug. That’s not a broad range. It’s a tight scientific window. If a generic fails this test, it doesn’t get approved.
The ANDA process: How generics get approved without full clinical trials
The pathway for generic drugs is called the Abbreviated New Drug Application, or ANDA. It was created by the Hatch-Waxman Act of 1984 to balance access and safety. Instead of proving a drug works from scratch, generic manufacturers show they’re pharmaceutically identical to a reference-listed drug (RLD) - the original brand-name version already approved by the FDA.
The ANDA review isn’t simple. It’s a deep dive into three areas:
- Bioequivalence data: Lab results showing how the drug behaves in the body - absorption, peak concentration, elimination. These aren’t theoretical; they’re based on real human studies.
- Labeling accuracy: The generic’s label must match the RLD exactly - same warnings, same dosing instructions, same contraindications.
- Manufacturing site inspection: Before approval, the FDA inspects the factory where the drug will be made. No inspection? No approval.
It used to take over two and a half years on average to approve a generic. That changed with the Generic Drug User Fee Amendments (GDUFA) in 2012. By letting the FDA collect fees from manufacturers, they hired more reviewers and improved their systems. Today, 95% of standard ANDAs are reviewed within 10 months - down from 30 months. That’s faster approval without cutting corners.
What happens inside a generic drug factory? The cGMP rules
Even if a drug works in a lab, it can fail in the real world if it’s made poorly. That’s why the FDA enforces Current Good Manufacturing Practices - or cGMP. These aren’t suggestions. They’re legal requirements.
Every generic manufacturer must have three core systems in place:
- Raw material control: Every ingredient - from the active pharmaceutical ingredient (API) to fillers and coatings - must be tested, traced, and stored properly. Contaminated materials? The whole batch is rejected.
- Process controls: Every step of production - mixing, drying, compressing, coating - has written procedures. Machines are calibrated. Temperatures are logged. Humidity is monitored. If a parameter goes outside the approved range, production stops.
- Lab testing: Finished tablets or capsules are tested for potency, dissolution rate, purity, and stability. Methods are validated. Results are audited. No shortcuts.
These rules apply whether the factory is in Ohio or India. The FDA doesn’t treat domestic and foreign plants differently - they’re held to the same standard. In 2021, the FDA conducted 1,082 inspections worldwide. About 74% of those met their performance goals. That number keeps climbing.

Foreign factories: The biggest challenge in oversight
More than 80% of generic drug ingredients and over 40% of finished products come from outside the U.S. That means the FDA has to inspect facilities in over 100 countries. It’s a massive logistical challenge.
In 2019, FDA inspections found quality issues in 15% of foreign facilities - compared to 8% in the U.S. That gap isn’t about intent. It’s about complexity. Some countries have less mature regulatory systems. Others have supply chains that are harder to trace.
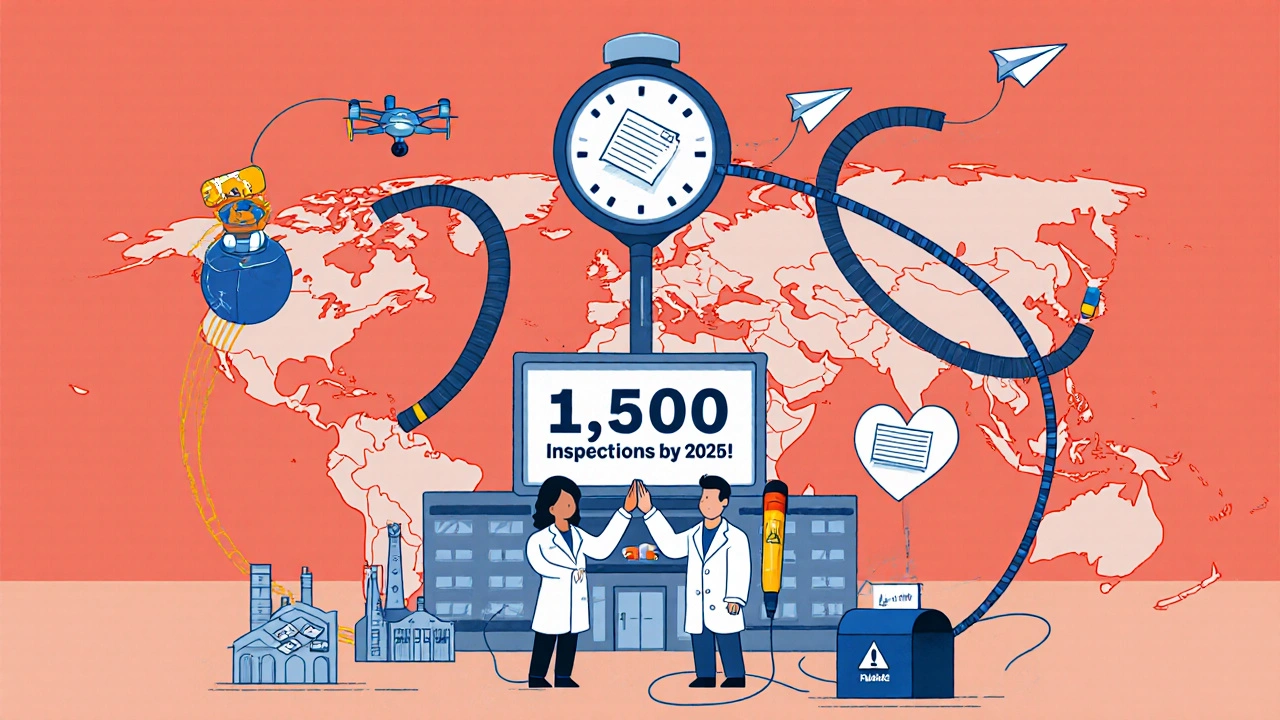
GDUFA III, launched in 2022, committed $1.1 billion through 2027 to fix this. One of its main goals: Increase foreign inspections from 1,082 in 2021 to 1,500 annually by 2025. The FDA now uses a risk-based system - focusing more on facilities with past violations, complex products, or high-volume production. It’s not random. It’s targeted.
What happens after approval? The FDA never stops watching
Approval isn’t the end. It’s just the beginning. The FDA keeps watching every generic drug on the market - from the moment it leaves the factory to when it’s taken by a patient.
Here’s how:
- MedWatch: Consumers and doctors can report side effects or problems through the FDA’s voluntary reporting system. In 2023, over 1.3 million reports were filed. The Division of Clinical Safety and Surveillance analyzes these to spot patterns - like if a certain generic is linked to more complaints than its brand-name version.
- Post-market studies: If a safety signal emerges, the FDA can require the manufacturer to run additional studies.
- Recalls and labeling updates: If a batch is contaminated or a warning is missing, the FDA can order a recall. They can also require updated labels or send "Dear Healthcare Provider" letters to alert doctors.
One example: In 2020, the FDA identified elevated levels of a cancer-causing impurity in some generic blood pressure meds. They didn’t wait for complaints. They proactively tested products, pulled affected batches, and worked with manufacturers to fix the process. That’s real-time oversight.
Who’s really in charge? The teams behind the scenes
The FDA doesn’t rely on one office. It’s a coordinated effort across multiple teams:
- Office of Generic Drugs (OGD): Reviews ANDAs and leads approval decisions.
- Office of Pharmaceutical Quality (OPQ): Oversees manufacturing standards, impurity controls, and facility inspections.
- Drug Safety Oversight Board (DSB): An independent panel of experts that advises the FDA on emerging safety issues.
- Clinical Safety and Surveillance Committee: A multidisciplinary team of doctors, chemists, and pharmacologists who review new safety signals for approved generics.
These teams don’t work in silos. They share data. They cross-check findings. If a lab in India flags an impurity, the safety team in Maryland is notified immediately. This system is designed to catch problems before they reach patients.
Why this matters: Real savings, real safety
Generic drugs save the U.S. healthcare system over $300 billion every year. That’s money that goes back to patients, insurers, and taxpayers. But that savings only works if the drugs are safe.
The FDA’s system isn’t perfect. There are still delays, inspection backlogs, and supply chain risks. But the improvements since 2012 are undeniable. Approval times are faster. Foreign inspections are increasing. Data systems are modernizing. The goal - stated clearly by former FDA Director Dr. Janet Woodcock - is simple: "Every generic drug on the U.S. market meets the same high standards of quality, safety, and efficacy as brand-name drugs."
That’s not marketing. It’s policy. And it’s working.
Are generic drugs as effective as brand-name drugs?
Yes. The FDA requires generic drugs to be bioequivalent to their brand-name counterparts, meaning they deliver the same amount of active ingredient into the bloodstream at the same rate. Studies show they work the same way in the body and have the same clinical outcomes. Thousands of patients use generics every day without any difference in effectiveness.
Why do generic drugs look different from brand-name ones?
Generic drugs can look different because U.S. law requires them to have a different shape, color, or marking than the brand-name version to avoid trademark infringement. But the active ingredient, strength, dosage form, and route of administration must be identical. The differences are only in non-medicinal components like dyes or fillers.
Can a generic drug cause different side effects than the brand?
The active ingredient is the same, so the side effect profile should be identical. However, inactive ingredients (like fillers or coatings) can sometimes cause allergic reactions in rare cases. If you notice new or different side effects after switching to a generic, report it to your doctor and to the FDA’s MedWatch program. The FDA tracks these reports to detect any unusual patterns.
How often does the FDA inspect generic drug factories?
The FDA aims to inspect all manufacturing facilities every two years. Domestic facilities are inspected more frequently than foreign ones, but the gap is shrinking. Under GDUFA III, the FDA plans to conduct 1,500 inspections annually by 2025, with priority given to high-risk facilities based on past compliance, product complexity, and supply chain data.
What happens if a generic drug fails an FDA inspection?
If a facility fails an inspection, the FDA can issue a warning letter, block approval of new products, or even refuse to import drugs from that site. In serious cases, the agency can issue an import alert, which means all products from that facility are automatically detained at the border until the issues are fixed. Manufacturers must correct the problems and pass a follow-up inspection before resuming production.
Are all generic drugs made overseas?
No. While over 80% of active pharmaceutical ingredients (APIs) come from outside the U.S., many finished generic drugs are still made domestically. The FDA inspects both U.S. and foreign facilities using the same standards. The location doesn’t determine safety - compliance with cGMP does.
How does the FDA decide which generics to inspect first?
The FDA uses a risk-based system. Facilities are ranked by factors like past inspection results, history of violations, complexity of the product (like inhalers or injectables), volume of production, and whether they supply critical medications. High-risk sites get inspected more often. This lets the FDA focus resources where they’re needed most.
Can I trust a generic drug if it’s much cheaper than the brand?
Yes. The lower price reflects lower development and marketing costs - not lower quality. Generic manufacturers don’t need to repeat expensive clinical trials, and they compete with each other, which drives prices down. The FDA’s approval and inspection process ensures that cost savings don’t come at the expense of safety or effectiveness.
What’s next for generic drug safety?
The FDA is moving toward real-time monitoring. New systems are being tested to track drug quality data as it’s generated - not just after the fact. That means quicker detection of contamination, impurities, or manufacturing errors.
They’re also expanding guidance for complex generics - like inhalers, patches, and injectables - that are harder to copy. The 2023 draft guidance on bioequivalence now covers over 2,800 drug products, up 40% since 2018. This helps manufacturers get it right the first time.
One thing won’t change: The FDA’s core promise. Every generic drug on the shelf must meet the same standard as the brand. No exceptions. No shortcuts. Just science, oversight, and accountability.
 Nov, 14 2025
Nov, 14 2025

Jennifer Walton
November 14, 2025 AT 06:06Kihya Beitz
November 14, 2025 AT 12:40Andrew Eppich
November 16, 2025 AT 04:35Jessica Chambers
November 16, 2025 AT 07:20Shyamal Spadoni
November 16, 2025 AT 10:09Ogonna Igbo
November 17, 2025 AT 19:04BABA SABKA
November 18, 2025 AT 15:57Chris Bryan
November 20, 2025 AT 11:13Jonathan Dobey
November 21, 2025 AT 06:25ASHISH TURAN
November 22, 2025 AT 16:02Ryan Airey
November 22, 2025 AT 16:17