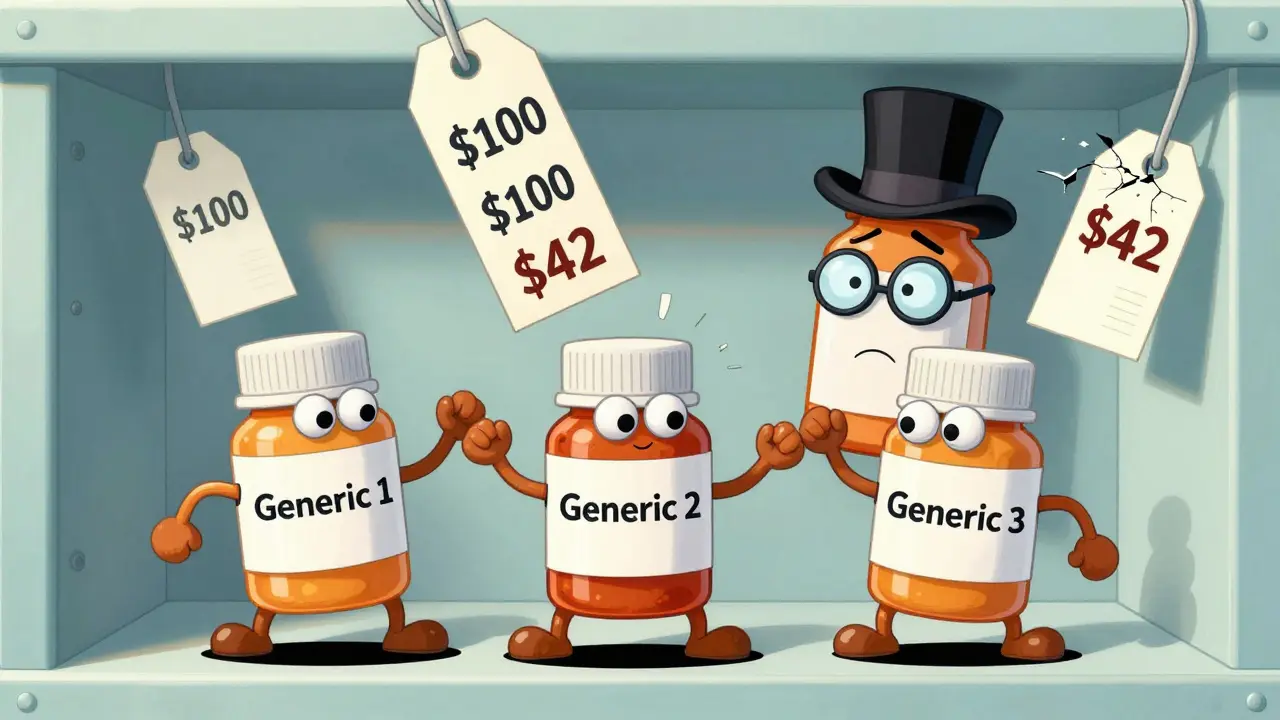
When a brand-name drug loses its patent, the first generic version usually hits the market at about 87% of the original price. That sounds like a big discount - until you see what happens when a second or third company starts making the same drug. Then prices don’t just drop. They plummet.
Why the second generic changes everything
The first generic drug maker doesn’t have much pressure to lower prices. They’re the only game in town, so they can charge close to what the brand did. But as soon as a second company gets FDA approval and starts selling the same pill, everything shifts. Suddenly, there are two suppliers. Two companies fighting for the same pharmacy, the same insurer, the same patient. That’s when prices start falling fast. According to FDA data from 2022, the second generic typically brings the price down to just 58% of the original brand price. That’s a 31% drop from the first generic’s price - all because one more company entered the market. It’s not magic. It’s basic economics: more sellers = lower prices. And this isn’t theoretical. It’s happening right now with common drugs like metformin, lisinopril, and atorvastatin.The third generic is where the real savings kick in
The third generic isn’t just another player - it’s the tipping point. Once three or more companies are making the same drug, prices don’t just dip. They crash. The FDA found that the third generic reduces the price to only 42% of the original brand price. That’s more than half off from the first generic’s price and nearly 60% off the brand’s original cost. This isn’t a one-time event. It’s a pattern. Markets with three or more generic manufacturers consistently see prices fall by 20% or more within three years. In larger markets - like those with over 15,000 monthly users - you often see eight, nine, or even ten different makers. In those cases, prices can drop 70-80% below the brand’s original price. For a drug that used to cost $100 a month, that means patients pay $20-$30 instead.What happens when competition disappears
The flip side of this story is just as important. When competition drops - when one company leaves the market or gets bought out - prices don’t stay low. They spike. A 2017 study from the University of Florida found that nearly half of all generic drug markets in the U.S. were stuck in duopolies - just two makers. In those cases, prices didn’t fall as much. And when one of those two companies pulled out or raised prices, the remaining one followed suit. Some drugs saw price jumps of 100% to 300% after competition shrank from three to two. That’s not a glitch. It’s how the system works when there’s not enough competition to keep prices in check. This is why the entry of the second and third generics matters so much. They’re not just options - they’re safeguards. They prevent any single company from holding the market hostage.
Why big wholesalers and PBMs make it harder
You might think more generics means lower prices for patients. And usually, it does. But there’s a catch: the middlemen. Three big wholesalers - McKesson, AmerisourceBergen, and Cardinal Health - control 85% of the generic drug supply chain. Three pharmacy benefit managers (PBMs) - Express Scripts, CVS Health, and Optum - handle 80% of prescription claims. These companies don’t always pass along the savings from generic competition to patients. Sometimes they keep the discount for themselves or use it to negotiate better deals with brand-name drug makers. That’s why you might see a big price drop on the manufacturer’s invoice, but your copay doesn’t change much. The gap between what the maker charges and what you pay at the pharmacy is often filled by markups from wholesalers and PBMs. The FDA found that when you look at manufacturer prices (what companies charge each other), the drop from multiple generics is steeper than what pharmacies actually pay. That’s because the middle layer is taking a bigger slice.How anti-competitive tactics block savings
Not all drug makers play fair. Some brand-name companies pay generic manufacturers to delay their entry. These are called “pay-for-delay” deals. The brand pays the generic company millions to sit on the sidelines instead of launching a cheaper version. The Blue Cross Blue Shield Association estimates this practice costs patients $3 billion a year in higher out-of-pocket costs. Others use “patent thicketing” - filing dozens of overlapping patents on minor changes to the drug, like a new coating or pill shape, just to delay generics. One drug had 75 patents filed to stretch its monopoly from 2016 to 2034. That’s not innovation. That’s legal obstruction. These tactics don’t just hurt patients. They hurt the entire system. The Actuarial Research Corporation estimates that removing these barriers could save the U.S. $1 trillion in drug spending over the next decade - mostly from faster entry of second and third generics.
What’s being done to fix it
There are signs of progress. The CREATES Act, passed in 2022, makes it harder for brand companies to block generic makers from getting the samples they need to test their drugs. The Preserve Access to Affordable Generics and Biosimilars Act targets pay-for-delay deals. And the FDA’s GDUFA III program, running from 2023 to 2027, is speeding up approvals for complex generics - the kind that usually take longer to enter the market. But the real leverage still comes from competition. Every new generic manufacturer that enters the market is a force multiplier. The FDA estimates that between 2018 and 2020, 2,400 new generic drugs saved patients $265 billion. That’s not because of regulation. It’s because more companies started making the same pills.What patients can do
You don’t need to wait for Congress or the FDA to act. If you’re on a generic drug, ask your pharmacist: “How many companies make this?” If there’s only one, ask if another version is available. Ask your doctor to write “dispense as written” on the prescription - that stops pharmacists from switching to the most expensive version just because it’s the default. Also, check your pharmacy’s price list. Some chains publish their cash prices for generics. You might find that the same drug costs $5 at one store and $40 at another. That’s not a mistake. It’s because one store is using a cheaper generic supplier. The bottom line? More competitors = lower prices. And the second and third generics are the most powerful tools we have to make drugs affordable. When they enter the market, they don’t just lower the price. They reset the entire system.Why do generic drug prices keep dropping after the first one enters the market?
Because each new generic manufacturer has to compete for the same customers - pharmacies, insurers, and patients. The first generic may charge close to the brand price, but the second and third need to undercut each other to win business. That drives prices down fast. By the time three companies are selling the same drug, prices often fall to 40% or less of the original brand cost.
Do all generic drugs get cheaper with more competitors?
Not always. Simple generics - like metformin or lisinopril - see big price drops with multiple makers. But complex generics, like inhalers or injectables, take longer to copy and have fewer manufacturers. In those cases, competition is limited, so prices stay higher. The FDA is working to speed up approvals for these harder-to-make drugs.
Why doesn’t my copay go down even though the drug is cheaper?
Your copay is set by your insurance plan, not by what the drug costs the pharmacy. PBMs and insurers often keep the savings from generic competition as profit or use it to negotiate lower prices on brand drugs. Even if the pharmacy paid $5 for the pill, your copay might still be $15 because your plan hasn’t updated its pricing structure.
What’s the difference between manufacturer price and pharmacy price for generics?
The manufacturer price is what the generic company charges the wholesaler. The pharmacy price is what the pharmacy pays after markups from wholesalers and PBMs. The FDA found that manufacturer prices drop much more sharply with competition than what pharmacies actually pay - because the middlemen absorb part of the savings.
Can I ask my pharmacist to switch to a cheaper generic version?
Yes - if your prescription doesn’t say "do not substitute." You can ask your pharmacist if there’s a lower-cost generic version available, even if your doctor prescribed a specific brand. Many pharmacies have lists of the cheapest generics they carry. Always check the price before you pay.
Are generic drugs as safe and effective as brand-name drugs?
Yes. The FDA requires all generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand. They must also meet the same strict standards for quality, purity, and performance. The only differences are in inactive ingredients - like color or filler - which don’t affect how the drug works.
What happens if only one company makes a generic drug?
When there’s only one manufacturer, prices stay high. There’s no competition to push prices down. In some cases, the single maker raises prices because they know patients have no alternatives. This is why having at least two or three manufacturers is critical - it prevents monopolies in the generic market.
 Dec, 15 2025
Dec, 15 2025
Jody Patrick
December 17, 2025 AT 11:47More generics? Good. But don't pretend this is about patients. It's about Wall Street wanting bigger margins and Pharma playing the long game. We're just the collateral damage.
Radhika M
December 17, 2025 AT 17:02Simple truth: more companies make same medicine = lower price. Like buying rice in bulk. First seller says $10, second says $7, third says $5. You win. No magic.
Raven C
December 19, 2025 AT 15:58How quaint. You invoke ‘basic economics’ as if Adam Smith himself had written the FDA’s 2022 report. The real tragedy is not the price drop-it’s the moral bankruptcy of reducing human health to a supply-chain spreadsheet.
Jigar shah
December 21, 2025 AT 12:55This is fascinating. I’ve seen this with metformin in India-when three local manufacturers entered, the price dropped from ₹120 to ₹18 per strip. The system works when competition isn’t stifled. But why do PBMs still control pricing so tightly?
Marie Mee
December 21, 2025 AT 22:43They're lying about the prices. The real story? The government lets Big Pharma own the patents and then lets the middlemen steal the savings. It's all rigged. You think your copay drops? Nah. They just move the money around. You're being played.
Naomi Lopez
December 23, 2025 AT 13:44It’s ironic that we celebrate market competition until it actually works-then we blame the system for not being ‘fair.’ If you want lower prices, don’t ask for regulation. Ask for more competitors. Simple.
Victoria Rogers
December 25, 2025 AT 12:32Third generic drives prices down? Sure. But only if the FDA doesn’t delay it for 18 months with ‘bioequivalence concerns.’ And don’t get me started on how the same companies that make brand drugs buy up the generics. It’s all one big oligopoly with different logos.
Jane Wei
December 26, 2025 AT 00:00So basically, if more companies make the same pill, you pay less. Who knew? 😅
Nishant Desae
December 26, 2025 AT 10:28I’ve been watching this for years, and honestly, it gives me hope. When I first started taking lisinopril, it was $45 a month. Now? $4. And it’s the exact same medicine. I know people who can’t afford their meds, and seeing this kind of change-real, tangible, patient-centered change-makes me believe we can fix this. It’s not perfect, but every new generic is a step toward dignity.
Philippa Skiadopoulou
December 26, 2025 AT 14:04Competition drives down prices. This is not novel. The real issue is transparency. If the manufacturer price is 40% of brand, why does the pharmacy charge 70%? The gap must be explained.
Jonathan Morris
December 28, 2025 AT 03:16Pay-for-delay? Patent thickets? These aren’t loopholes. They’re criminal enterprises disguised as IP law. And the FDA? They’re asleep at the wheel. This system isn’t broken-it was designed this way.
Linda Caldwell
December 29, 2025 AT 08:59More generics = more power to the people. Every time a new company enters, someone’s life gets easier. Keep pushing. Keep asking. Keep checking prices. You’re not just saving money-you’re fighting back.
Anna Giakoumakatou
December 30, 2025 AT 02:21Oh, so now we’re celebrating capitalism’s ‘efficiency’? How poetic. The same system that priced insulin at $300 a vial now gets a gold star for letting you buy metformin for $3. What a world we live in.
CAROL MUTISO
December 30, 2025 AT 13:38It’s beautiful, really-the way market forces, when unchained from greed, can turn a life-saving drug from a luxury into a right. But let’s not pretend the system is innocent. The real heroes aren’t the FDA or Congress. They’re the scrappy little labs in Hyderabad and Bangalore that refused to wait for permission to save lives.