Key Takeaways
- Major Depressive Disorder (MDD) raises the risk of heart disease, diabetes, and chronic pain.
- Stress hormones like cortisol disrupt sleep, appetite, and immune function.
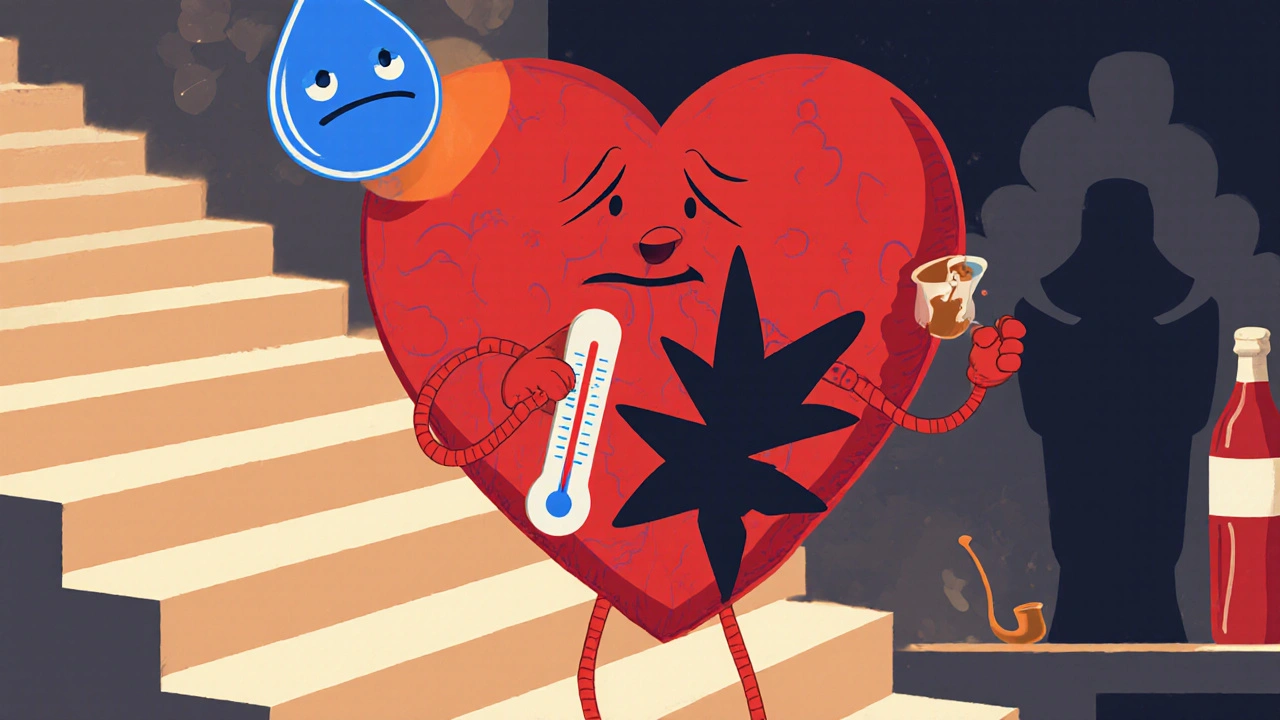
- Unhealthy coping habits-smoking, alcohol, inactivity-exacerbate physical decline.
- Early screening and coordinated care can cut the odds of serious complications.
- Small lifestyle tweaks (movement, sleep hygiene, nutrition) make a measurable difference even while depressed.
When Major Depressive Disorder is a common mental health condition marked by persistent low mood, loss of interest, and cognitive changes, its impact reaches far beyond feelings of sadness. It can reshape Physical Healththe overall functioning of the body’s systems, from heart and metabolism to immunity and pain perception in ways many people don’t expect. Below we break down the science, the everyday signs, and the steps you can take to protect your body while navigating depression.
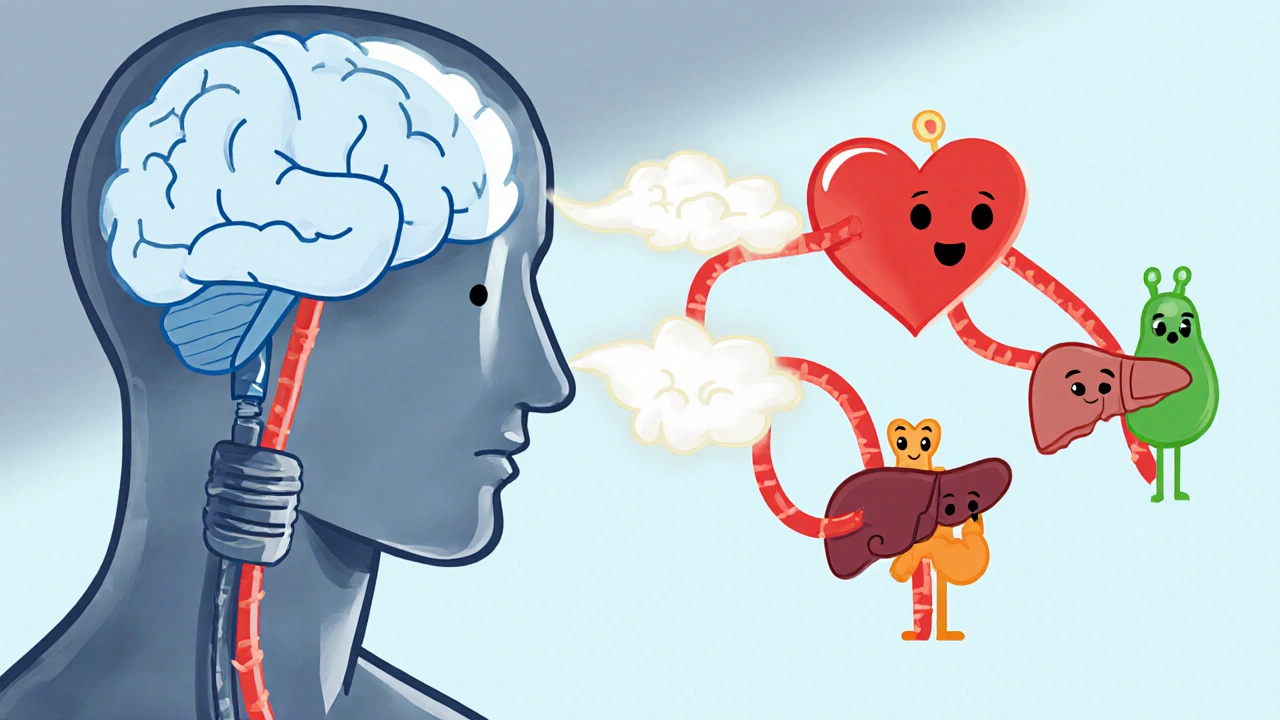
How Depression Touches Every Body System
Think of the body as a network of inter‑linked circuits. When one circuit-your mood center-stays stuck in a low‑power mode, the others start to wobble. Here are the main pathways:
- Neuro‑endocrine route: The brain releases more cortisol, the “stress hormone,” which spikes blood sugar and raises blood pressure.
- Autonomic imbalance: Depression often tilts the balance toward sympathetic (fight‑or‑flight) activity, leaving the parasympathetic (rest‑and‑digest) side under‑worked.
- Behavioural changes: Poor sleep, reduced activity, and unhealthy eating become the norm, feeding back into physiological stress.
These mechanisms explain why a diagnosis of MDD is a red flag for many chronic illnesses.
Cardiovascular Disease: The Silent Partner
Heart disease is the leading cause of death worldwide, and depression sits on its tail. A 2023 meta‑analysis of 28 longitudinal studies (over 1.2 million participants) found that people with MDD have a 1.5‑times higher risk of developing coronary artery disease compared with those who never experienced a depressive episode.
The link isn’t just behavioural-smoking and inactivity certainly matter-but also biological. Elevated cortisol and inflammatory markers (like C‑reactive protein) stiffen blood vessels, making plaques more likely to form. In everyday terms, a person with depression may notice a quicker onset of chest tightness after climbing stairs or an increased palpitations during stressful moments.
Metabolic Syndrome, Obesity, and Diabetes
Metabolic syndrome is a cluster of conditions-high blood pressure, excess abdominal fat, insulin resistance, and abnormal cholesterol-that together spike heart‑attack and stroke risk. Depression both predicts and worsens this cluster.
Research from the UK Biobank (2022) showed that individuals with persistent depressive symptoms were 30 % more likely to develop type 2 diabetes over ten years. The culprit? Cortisol drives gluconeogenesis, raising blood glucose, while emotional eating pushes calorie intake upward. Sleep disturbances also impair insulin sensitivity, creating a perfect storm.
If you’ve noticed a gradual weight gain despite unchanged diet, or you’re waking up feeling groggy and thirsty, it could be your hormones screaming for help.
Immune System Dysregulation
Depression isn’t just a brain thing; it’s a whole‑body inflammatory response. Studies measuring cytokines (the body’s pain‑signalling proteins) consistently find higher levels of interleukin‑6 (IL‑6) and tumor necrosis factor‑alpha (TNF‑α) in people with MDD.
What does that mean for you? A weaker ability to fight off infections, slower wound healing, and a higher chance of autoimmune flare‑ups. For example, a 2021 cohort of rheumatoid arthritis patients with comorbid depression required 20 % higher medication doses to achieve the same disease control.
Chronic Pain and Sleep Disturbances
It’s common to hear, “My back hurts because I’m depressed.” The relationship goes both ways. Persistent pain raises cortisol, which deepens depressive feelings, while depression lowers the brain’s natural pain‑modulating chemicals (like endorphins).
Sleep is another two‑way street. Insomnia is a diagnostic criterion for MDD, yet poor sleep also fuels depressive cognition. A 2024 sleep‑lab study found that depressed participants spent 20 % less time in deep (slow‑wave) sleep, which is critical for cellular repair and hormone regulation.
Practical tip: Keep a simple sleep diary for a week-note bedtimes, wake times, and any nighttime awakenings. Patterns often reveal where to intervene.
Unhealthy Coping: Substance Use, Smoking, and Inactivity
When mood dips, many turn to quick fixes. Alcohol, nicotine, and high‑sugar foods provide fleeting relief but aggravate physical health.
- Alcohol: Heavy drinking spikes triglycerides and can worsen liver function, especially in people already battling metabolic syndrome.
- Smoking: Depressed smokers have a 40 % higher mortality risk than non‑smokers with the same diagnosis.
- Physical inactivity: Exercise releases endorphins, but depression can sap motivation. Sedentary behaviour accelerates muscle loss and impairs cardiovascular fitness.
Addressing these habits early reduces the compounding effect on both mind and body.

Putting It All Together: Managing Physical Health While Depressed
Great news: you don’t need a miracle cure to lower the physical toll of depression. A coordinated plan that tackles mood, lifestyle, and medical monitoring works best.
1. Ask for a Physical Health Check‑up
When you receive an MDD diagnosis, request a baseline panel: blood pressure, fasting glucose, lipid profile, and an inflammatory marker (CRP). Knowing where you stand gives both you and your clinician a roadmap.
2. Integrate Treatment Modalities
Therapy and medication each play a role. Some antidepressants (e.g., SSRIs) have neutral or even favourable effects on weight and blood pressure, while others might increase appetite. Discuss options with your prescriber.
3. Move, Even If It Feels Hard
Start small: a 10‑minute walk after breakfast, or a short stretching routine while watching TV. Gradual activity improves insulin sensitivity, lowers cortisol, and boosts mood within weeks.
4. Prioritise Sleep Hygiene
Set a consistent bedtime, dim lights an hour before sleep, and limit caffeine after noon. If insomnia persists, cognitive‑behavioral therapy for insomnia (CBT‑I) is a proven, medication‑free solution.
5. Nutrition Basics
Eat a balanced plate-lean protein, whole grains, plenty of vegetables, and healthy fats (like olive oil or avocado). Limit added sugars and processed foods, which can spike blood glucose and worsen mood swings.
6. Monitor and Adjust
Schedule follow‑up labs every 6‑12 months. If you notice new chest pain, unexplained weight change, or persistent fatigue, flag it quickly-early intervention prevents complications.
Risk Comparison Table
| Condition | Risk Increase (vs. non‑depressed) | Typical Timeframe |
|---|---|---|
| Coronary artery disease | 1.5 × | 5-10 years |
| Type 2 diabetes | 1.3 × | 7-12 years |
| Stroke | 1.4 × | 4-9 years |
| Obesity (BMI ≥ 30) | 1.6 × | 2-5 years |
| Chronic pain syndromes | 1.8 × | 1-3 years |
| Immune‑related disorders | 1.2-1.4 × | Varies |
Frequently Asked Questions
Can antidepressants worsen physical health?
Most modern antidepressants are metabolically neutral, but a few (like certain tricyclics) can affect weight or blood pressure. Your doctor can choose a medication that aligns with any existing health concerns.
How soon will lifestyle changes impact my risk?
Even modest increases in activity (e.g., 30 minutes of brisk walking) can lower cortisol within weeks and improve insulin sensitivity in a few months. Consistency beats intensity when depression saps motivation.
Is there a link between depression and cancer?
The evidence is mixed. Some studies suggest depressed individuals may delay cancer screening, leading to later-stage diagnoses. The direct biological link remains less clear than with heart disease or diabetes.
Should I get screened for heart disease if I’m depressed?
If you have risk factors-family history, high blood pressure, or smoking-a cardiovascular check‑up is advisable. Talk to your GP about adding a lipid panel and ECG to your routine labs.
Can therapy improve my physical health?
Yes. Cognitive‑behavioral therapy often includes behavioral activation, which nudges you toward regular exercise and healthier eating-both of which lower physical disease risk.
Understanding that Major Depressive Disorder reaches into the body’s core systems empowers you to act early. By pairing mental‑health treatment with simple, evidence‑based lifestyle steps, you can blunt the physical blow and keep both mind and body on a steadier path.
 Sep, 28 2025
Sep, 28 2025
Selina M
September 28, 2025 AT 08:19Hey folks, great rundown on how depression messes with ur body. Keep it simple – move a lil each day, drink water, and try to get some sunlight when u can. Small steps add up big.
Nicholai Battistino
October 11, 2025 AT 12:59This is solid info, thanks.
Suraj 1120
October 24, 2025 AT 17:39Look, the article glosses over the fact that many of these stats come from studies that cherry‑pick participants. You can't just blame cortisol for every heart attack; genetics and environment play huge roles. Also, the advice to 'just walk 10 minutes' feels condescending to people whose depression is severe enough to make any movement feel impossible. The piece should mention that pharma incentives often drive these lifestyle recommendations, not pure science. Overall, it’s a decent primer but it’s missing nuance.
Shirley Slaughter
November 6, 2025 AT 21:19I hear you, Suraj. Depression can feel like a shadow that seeps into every organ, but the good news is that even tiny habits can light a spark. Think of a morning stretch as a gentle sunrise for your nervous system, or a short walk as a tide that washes away stale stress hormones. Remember, you’re not alone in this battle, and every supportive hand counts.
Sean Thomas
November 20, 2025 AT 01:59What they don’t tell you is that big pharma loves keeping depression around – the more meds they sell, the more they can push their 'lifestyle' agendas that distract us from real cures. They fund half the ‘research’ that links cortisol to heart disease, while ignoring studies that show natural immunity can reverse those risks. Stay skeptical.
Aimee White
December 3, 2025 AT 06:39Ah, the grand tapestry of hidden agendas! Imagine a world where pharmaceutical titans sprinkle micro‑doses of melancholia in our water supply, just enough to keep us hooked on their shiny pills. Then they sell us glittering wellness apps and ‘exercise plans’ that funnel our data straight to their vaults. It’s a narrative straight out of a cyber‑noir novel, yet the statistics keep humming the same tune.
Javier Muniz
December 16, 2025 AT 11:19Yo, thanks for breaking this down. Real talk: start with something doable, like a quick dance to your favorite song while you wait for the coffee. It’ll boost endorphins and give your heart a tiny workout without feeling like a gym session. Keep it chill and celebrate each little win.
Sarah Fleming
December 29, 2025 AT 15:59Indeed, Javier. The truth is that elite circles have known for decades that the mind–body nexus can be harnessed to control populations. They employ curated ‘wellness’ programs as a veneer, while covertly monitoring biometric data to predict dissent. Only a cultivated few see through the façade.
Debra Johnson
January 11, 2026 AT 20:39It is incumbent upon us, as responsible citizens, to recognize that the propagation of complacent narratives regarding mental health and physical disease-while convenient for profit‑driven entities-is ethically indefensible; we must demand transparency, rigorous peer review, and equitable access to preventive care, lest we perpetuate a system that values economic gain over human flourishing.
Andrew Wilson
January 25, 2026 AT 01:19Yo, that's the truth-if we keep buying into these half‑baked health hacks, we're just feeding the same greedy machine; we gotta call them out and push for real science, not just feel‑good fluff.
Kristin Violette
February 7, 2026 AT 05:59From a biopsychosocial perspective, integrating psychopharmacology with lifestyle medicine yields a synergistic effect on allostatic load; thus, clinicians should employ a multimodal framework that includes behavioral activation, nutritional psychiatry, and circadian rhythm optimization to attenuate the inflammatory cascade associated with major depressive disorder.
Theo Asase
February 20, 2026 AT 10:39Listen up, because what they’re selling you in glossy health magazines is nothing more than a sophisticated neuro‑psychological smokescreen.
The moment you accept that a simple walk can ‘fix’ cortisol spikes, you hand over your autonomy to an industry that profits from chronic dependency.
These so‑called ‘evidence‑based’ guidelines are drafted behind closed doors by committees funded by the very corporations whose bottom line hinges on you staying under perpetual medical supervision.
They meticulously cherry‑pick data that supports their narrative while discarding any research that shows natural resilience can reverse metabolic damage.
Meanwhile, secret think tanks commissioned by defense contractors are mapping the neuro‑immune pathways to develop bio‑feedback weapons that can subtly destabilize entire populations.
It’s no coincidence that spikes in depression rates align with the rollout of digital health platforms that harvest your biometric signatures.
Your heart rate variability, sleep architecture, and even gut microbiome profiles are being logged, analyzed, and sold to the highest bidder.
This data is then used to fine‑tune targeted advertising that nudges you toward prescribed supplements and overpriced wellness retreats.
In the grand scheme, the goal is not health restoration but the creation of a docile, data‑rich workforce that can be steered with algorithmic precision.
When you read about ‘small lifestyle tweaks,’ understand that it is a euphemism for micro‑interventions that keep you constantly engaged with monitoring devices.
The narrative of personal responsibility conveniently diverts attention from the systemic manipulation at play.
If you truly want to reclaim your physiological sovereignty, you must reject the one‑size‑fits‑all protocols and seek out community‑driven, low‑tech practices that can’t be commodified.
Rediscovering ancestral movement patterns, seasonal fasting, and communal storytelling reactivates innate healing pathways that modern medicine has tried to suppress.
Do not be fooled by the polished graphics and celebrity endorsements that mask a deeper agenda.
The battle for your mind and body is being waged on a battlefield of data, patents, and political lobbying.
Stay vigilant, question every ‘expert’ opinion, and remember that true health is a collective right, not a market commodity.
Only then can we dismantle the hidden scaffolding that sustains this grand health illusion.