Calcitriol-PTH Clinical Scenario Calculator
This tool helps you visualize the relationships between calcitriol, parathyroid hormone (PTH), calcium levels, and clinical signs in different endocrine conditions. Select a condition from the dropdown to see expected values.
Select a condition to view details
Choose a clinical scenario from the dropdown above to see expected hormone levels and clinical signs.
Ever wondered why a tiny molecule called calcitriol is often called the “active” form of vitamin D? It’s the hormone that talks to your parathyroid glands, tells your bones when to grow, and even nudges your immune system. In this guide we’ll walk through exactly how calcitriol influences parathyroid hormone (PTH) and what that means for overall endocrine health. By the end you’ll see the feedback loop, the organs involved, and the clinical clues that signal something’s off.
What is Calcitriol and How Is It Made?
Calcitriol, chemically known as 1,25-dihydroxyvitamin D₃, is the most potent metabolite of vitamin D. The journey starts when skin‑produced cholecalciferol (vitamin D₃) or dietary ergocalciferol (vitamin D₂) travels to the liver, where 25-hydroxylase converts it into 25‑hydroxyvitamin D (25‑OH D). This precursor circulates bound to vitamin D‑binding protein. The final activation step occurs in the kidney specifically the proximal tubule cells where the enzyme 1‑alpha hydroxylase (CYP27B1) adds a second hydroxyl group, creating calcitriol. Hormonal signals - low calcium, low phosphate, and high PTH - up‑regulate this enzyme, while fibroblast growth factor‑23 (FGF‑23) and high calcitriol itself can tone it down.
The PTH‑Calcitriol Feedback Loop
Parathyroid hormone, secreted by the four tiny parathyroid glands on the thyroid, is the primary regulator of blood calcium. When calcium drops, PTH spikes. One of PTH’s key actions is to boost renal 1‑alpha hydroxylase, which raises calcitriol levels. In turn, calcitriol works back on the parathyroids: it binds to the vitamin D receptor (VDR) a nuclear receptor present in parathyroid cells and suppresses PTH gene transcription. This negative feedback helps prevent runaway calcium elevation. Think of it as a thermostat: PTH turns the heat on, calcitriol senses the temperature and nudges the thermostat down.
Calcium and Phosphate Balance: The Core of the System
Calcitriol’s most visible job is to improve intestinal absorption of calcium and phosphate. In the intestine especially the duodenum and jejunum where calcium channels and transporters are expressed, it up‑regulates the expression of TRPV6 (a calcium channel) and calbindin‑D9k (a binding protein), boosting the amount of mineral that crosses into the bloodstream. Simultaneously, calcitriol enhances phosphate transport via NaPi‑IIb. When enough calcium and phosphate enter circulation, PTH secretion eases, completing the loop.
Bone Remodeling: Osteoblasts, Osteoclasts, and the Balance of Growth
Bone isn’t static; it’s a living tissue constantly being broken down by osteoclasts large multinucleated cells that resorb bone matrix and rebuilt by osteoblasts cells that lay down new bone matrix and eventually become osteocytes. Calcitriol influences both sides. By increasing serum calcium, it indirectly reduces osteoclast activation because PTH‑driven osteoclastogenesis wanes. Directly, calcitriol binds VDR on osteoblasts, prompting them to produce RANKL, a molecule that can still stimulate osteoclasts when needed. The net effect is a finely tuned balance: enough resorption to remodel, enough formation to maintain strength.

Beyond Calcium: Wider Endocrine and Immune Effects
Calcitriol isn’t just a calcium manager. It reaches into several endocrine pathways:
- Renin‑angiotensin system: VDR activation in the kidney suppresses renin expression, modestly lowering blood pressure.
- Immune modulation: In immune cells, calcitriol skews T‑cell responses toward a regulatory phenotype, reducing inflammation.
- Pancreatic function: VDR in beta‑cells supports insulin secretion, linking vitamin D status with glucose control.
Because these systems intersect with calcium handling, disturbances in calcitriol can ripple through the whole endocrine network.
Clinical Snapshots: When the System Gets Out of Sync
Understanding the biochemistry pays off when you see patients:
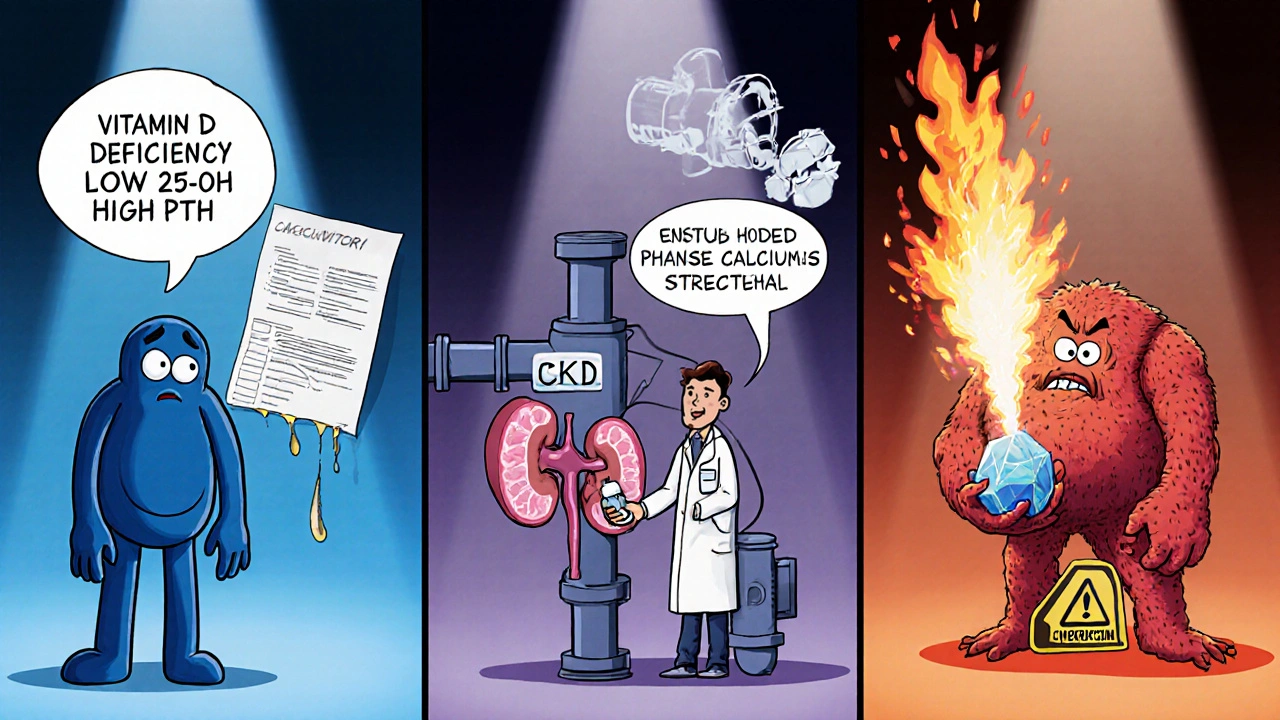
- Vitamin D deficiency (low 25‑OH D) limits calcitriol production, leading to secondary hyperparathyroidism - high PTH, low‑normal calcium, bone demineralization, and muscle weakness.
- Chronic kidney disease (CKD) reduces 1‑alpha hydroxylase activity, causing low calcitriol despite normal 25‑OH D. PTH shoots up, driving renal osteodystrophy.
- Granulomatous diseases (sarcoidosis, tuberculosis) feature macrophage‑derived 1‑alpha hydroxylase, which can overproduce calcitriol, suppressing PTH and causing hypercalcemia.
- Genetic VDR mutations blunt calcitriol’s signaling, resulting in rickets‑like bone disease even with adequate vitamin D levels.
Lab work‑up usually includes serum calcium, phosphate, PTH, 25‑OH D, and if needed, calcitriol itself. Imaging may reveal bone density loss or nephrocalcinosis in hypercalcemia cases.
Practical Tips: Monitoring, Supplementing, and Lifestyle
If you’re caring for yourself or patients, keep these points in mind:
- Target a 25‑OH D level of 30‑50 ng/mL for most adults. This range usually yields sufficient calcitriol without excess.
- When PTH is elevated and calcium is low‑normal, consider a vitamin D supplement (cholecalciferol 1000‑2000 IU daily) and re‑check in 8‑12 weeks.
- For CKD stages 3‑5, active vitamin D analogs (calcitriol or alfacalcidol) are often prescribed because the kidneys can’t finish the activation step.
- Watch for hypercalcemia signs (polyuria, fatigue, stones) if you’re on high‑dose calcitriol or have granulomatous disease.
- Include calcium‑rich foods (dairy, fortified plant milks, leafy greens) and moderate sun exposure to support the whole pathway.
Regular monitoring of calcium, phosphate, and PTH helps catch imbalances early and adjusts dosing before complications arise.
Key Takeaways
- Calcitriol is the active hormone that closes the loop between calcium intake, intestinal absorption, and parathyroid hormone release.
- Low calcium → PTH ↑ → kidneys make more calcitriol → calcitriol suppresses PTH via VDR.
- Both deficiency and excess of calcitriol disrupt bone health, kidney function, and even blood pressure.
- Clinical clues: secondary hyperparathyroidism in vitamin D deficiency, suppressed PTH with high calcium in granulomatous disease.
- Maintain adequate 25‑OH D levels, monitor labs, and adjust supplementation based on kidney function and disease state.
Comparison Table: Hormone Levels and Expected Effects
| Condition | Calcitriol | PTH | Serum Calcium | Typical Clinical Sign |
|---|---|---|---|---|
| Vitamin D Deficiency | Low | High | Low‑Normal | Bone pain, muscle weakness |
| CKD‑Associated Low Calc | Low | High | Low‑Normal | Renal osteodystrophy |
| Granulomatous Disease | High | Suppressed | High | Hypercalcemia, kidney stones |
| Optimal Vitamin D Status | Normal | Normal | Normal | Stable bone turnover |
Frequently Asked Questions
What is the difference between calcitriol and vitamin D supplements?
Vitamin D supplements (cholecalciferol or ergocalciferol) are precursors that need liver and kidney activation. Calcitriol is the final, active hormone and is usually given only when the kidneys can’t make it, such as in advanced CKD or certain genetic disorders.
Can high calcium intake lower PTH without calcitriol?
Yes. Raising serum calcium directly signals the parathyroids to reduce PTH. However, without calcitriol the gut absorption of that calcium is limited, so the effect is modest compared to the hormone‑driven pathway.
Why do patients with sarcoidosis develop hypercalcemia?
Macrophages in granulomas express 1‑alpha hydroxylase, converting 25‑OH D to calcitriol uncontrollably. The excess calcitriol boosts intestinal calcium absorption and suppresses PTH, leading to high calcium levels.
Do I need to test calcitriol levels routinely?
Usually not. Most labs start with 25‑OH D, calcium, phosphate, and PTH. Calcitriol testing is reserved for complex cases like CKD, granulomatous disease, or when treatment with active vitamin D is considered.
Can vitamin D toxicity affect PTH?
Excessive calcitriol (or very high 25‑OH D) can suppress PTH dramatically, sometimes causing hypocalcemia if calcium intake isn’t sufficient. Symptoms include nausea, weakness, and paradoxical bone pain.
 Oct, 20 2025
Oct, 20 2025
Michael Kusold
October 20, 2025 AT 13:21calcitrol flips the switch on calcium absorption, no joke.
Jeremy Lysinger
October 25, 2025 AT 04:27The PTH‑calcitriol feedback loop is one of the most elegant control systems in the body.
When serum calcium dips, the parathyroids release PTH, which rushes to the kidneys and tells the 1‑alpha hydroxylase to crank out more calcitriol.
That extra calcitriol promptly boosts calcium absorption in the gut, nudging serum calcium back toward normal.
At the same time, calcitriol binds to vitamin D receptors on the parathyroid cells and tells them to tone down PTH gene transcription.
This double‑hit prevents the system from overshooting, much like a thermostat that both heats and cools.
If you look at patients with vitamin D deficiency, you’ll see a classic picture of high PTH, low‑normal calcium, and bone pain.
The kidneys try to compensate by making as much calcitriol as they can, but without enough substrate the loop stalls.
In chronic kidney disease the final activation step is crippled, so even with adequate 25‑OH D the active hormone stays low.
That’s why you often need prescription calcitriol or analogs for those folks.
On the flip side, granulomatous diseases like sarcoidosis give macrophages their own 1‑alpha hydroxylase, flooding the bloodstream with calcitriol.
The result is suppressed PTH, high calcium, and sometimes kidney stones.
Managing those cases means tempering the extra vitamin D production, not just cutting dietary calcium.
The interplay also reaches the renin‑angiotensin system, where calcitriol can dampen renin expression and modestly lower blood pressure.
In the immune arena, it steers T‑cells toward a regulatory phenotype, which may explain why low vitamin D status is linked to autoimmunity.
So when you assess endocrine health, think of calcitriol as the hub that ties calcium, bone, kidney, blood pressure, and immunity together.
Nelson De Pena
October 29, 2025 AT 18:34Calcitriol’s ability to suppress PTH hinges on its interaction with the vitamin D receptor in the parathyroid glands, and that mechanism is dose‑dependent.
Higher levels of the hormone produce a more pronounced transcriptional shut‑down of the PTH gene.
Clinically, you’ll see a gradual PTH decline as 25‑OH D rises above the 30 ng/mL threshold, assuming calcium intake is adequate.
In patients with renal impairment, however, the same rise doesn’t occur because the kidney can’t perform the final hydroxylation step.
Wilson Roberto
November 3, 2025 AT 09:41Think of calcitriol as a quiet philosopher whispering to every cell that balances minerals.
It doesn’t just shout about calcium; it subtly nudges blood pressure and immune tolerance.
That’s why a deficiency can feel like a cascade of unrelated symptoms, yet they’re all tied to the same silent regulator.
Narasimha Murthy
November 8, 2025 AT 00:47While the overview is solid, it overlooks the fact that not all patients respond uniformly to supplementation; genetic variations in the VDR can blunt the expected feedback.
Samantha Vondrum
November 12, 2025 AT 15:54Thank you for the comprehensive synthesis.
From a clinical teaching perspective, emphasizing the threshold values for 25‑OH D and the role of active analogs in CKD is especially valuable.
Please continue to integrate such nuanced guidance in future posts.
Kelvin Egbuzie
November 17, 2025 AT 07:01Sure, the “active” form is just a pawn in the grand pharma scheme-big pharma loves to push calcitriol analogs to keep us hooked on pills.
Katherine Collins
November 21, 2025 AT 22:07Lol, maybe the real conspiracy is how we keep forgetting to get sun! 😜
Taylor Nation
November 26, 2025 AT 13:14Great points all around.
Just a reminder to pair vitamin D supplementation with adequate dietary calcium, otherwise the hormone can’t do its job effectively.
Also, keep an eye on phosphate levels in CKD patients; they’re often the hidden culprit.
Nathan S. Han
December 1, 2025 AT 04:21The drama of calcium, phosphate, and hormones is truly theatrical!
When calcitriol takes center stage, the parathyroids bow out, and the bones either applaud or crumble, depending on the script you’ve written with nutrition and kidney function.
Ed Mahoney
December 5, 2025 AT 19:27Oh sure, let’s all become endocrinology professors after reading a blog post. 🙄
Brian Klepacki
December 10, 2025 AT 10:34Behold, the saga of calcitriol-a tale of micronutrients that could rival any Shakespearean tragedy, if only the masses would appreciate the nuance.
Shermaine Davis
December 15, 2025 AT 01:41Nice summary! I learned why I need more milk and sunshine.