Medication Safety Checker for Seniors
This tool checks if a medication is listed in the Beers Criteria—the official list of medications that pose unacceptable risks for people over 65. Enter a medication name below to see its risk level and why it might be dangerous for seniors.
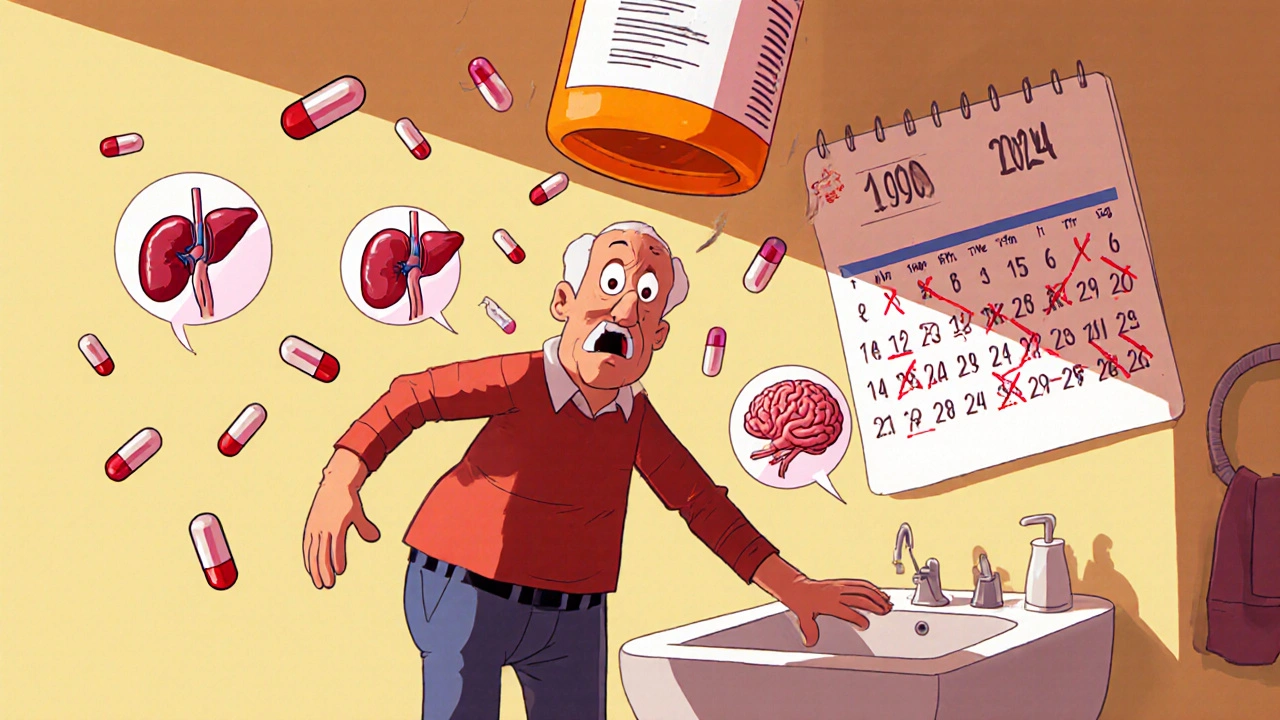
When you’re 80, a pill that helped you at 50 might leave you dizzy, confused, or even hospitalized. It’s not that the medicine changed. It’s that your body did. As we age, how our bodies handle medications shifts in ways most people don’t expect-and doctors don’t always adjust for. Older adults are more than twice as susceptible to side effects as younger people, and nearly one in three hospital visits for seniors are tied to medications that could’ve been avoided.
Why Older Bodies React Differently to Medicines
Your body’s ability to process drugs changes with age. It’s not just about being "slower." It’s about physical changes that alter how drugs move through you, how long they stay, and how strongly they hit.- Water content drops by about 15% between age 25 and 80, while body fat increases. That means water-soluble drugs like lithium build up too much, and fat-soluble drugs like diazepam stick around longer.
- Your kidneys filter blood less efficiently. After 40, your glomerular filtration rate drops by about 0.8 mL/min per year. Drugs cleared by the kidneys-like digoxin, antibiotics, and pain meds-can accumulate to dangerous levels if doses aren’t lowered.
- Your liver processes drugs more slowly. Blood flow to the liver drops 20-40% by age 65. That affects drugs like propranolol and verapamil, which rely on liver metabolism to break down.
- Protein levels in your blood fall, especially albumin. That means more of a drug like warfarin floats around freely in your bloodstream, making it stronger than expected-even at the same dose.
What Medications Are Riskiest for Seniors?
Some drugs are simply too dangerous for older adults-even at low doses. The Beers Criteria, updated every two years by the American Geriatrics Society, lists 56 medications that pose unacceptable risks for people over 65. These aren’t obscure drugs. Many are common.- Anticholinergics like diphenhydramine (Benadryl) and oxybutynin: These cause confusion, memory loss, and delirium. A 2023 University of Florida study found people over 75 were 4.2 times more likely to have delirium from these drugs than younger adults.
- Benzodiazepines like lorazepam and alprazolam: These increase fall risk by 2-3 times. Hip fractures from falls linked to these drugs cost the U.S. over $1 billion annually.
- NSAIDs like ibuprofen and naproxen: They raise the risk of stomach bleeds and kidney failure. One study found 1 in 4 seniors on daily NSAIDs had signs of kidney damage within 6 months.
- Antidepressants like amitriptyline: These cause urinary retention, especially in men with enlarged prostates. One Reddit user at 78 needed a catheter after starting it for nerve pain.
- Antihypertensives like doxazosin: These cause dangerous drops in blood pressure when standing. A 2022 JAMA study found 28% of people over 80 had symptoms like dizziness or fainting-compared to just 9% of those aged 50-65.
Polypharmacy: When More Medicines Mean More Danger
Nearly half of all adults over 65 take five or more prescription drugs each month. One in five take ten or more. This isn’t just a number-it’s a ticking time bomb. When you’re on multiple medications, the chances of harmful interactions rise sharply. One drug can slow how another is broken down. Another might make your kidneys work harder. Add over-the-counter pills, supplements, or herbal remedies-and the mix becomes unpredictable. A 2022 JAMA study found that when pharmacists did a "Brown Bag Review"-where patients brought all their meds to an appointment-they found an average of 3.2 errors per person. That includes duplicates, wrong doses, or drugs that shouldn’t be taken together. And here’s the worst part: Many of these drugs were prescribed years ago for conditions that no longer matter. A blood pressure pill for a 60-year-old might still be on the list at 82, even though the patient’s BP is now normal. Or a sleep aid from 2015 is still being refilled, even though the patient hasn’t slept poorly in a year.
How Doctors Should Adjust Dosing-And Why They Often Don’t
The rule of thumb for older adults is simple: Start low, go slow. That means beginning at 25-50% of the standard adult dose and increasing only if needed-and only after weeks, not days. But in practice? Many doctors still prescribe the same doses they use for 50-year-olds. One caregiver on AgingCare.com shared that her 82-year-old mother fractured her hip after being prescribed a standard blood pressure dose. The doctor hadn’t adjusted it for her age or kidney function. Why does this happen?- Most clinical trials exclude people over 75. So doctors don’t have solid data on what doses are safe.
- Time constraints in appointments mean quick scripts, not careful reviews.
- Many providers aren’t trained in geriatric pharmacology. Only 72% of U.S. medical schools now teach it regularly.
What Seniors and Families Can Do
You don’t have to wait for your doctor to bring it up. Here’s what you can do today:- Bring every pill, capsule, and supplement to your next appointment-yes, even the ones you only take "when needed." Use a brown bag.
- Ask: "Is this drug still necessary? Could it be causing my dizziness or confusion?"
- Request a kidney function test (eGFR) if you’re on any drug cleared by the kidneys.
- Check if your meds are on the Beers Criteria list. The free mobile app is updated yearly and used by over 125,000 clinicians.
- If you’ve had a fall, memory lapse, or unexplained weight loss, ask: "Could a medication be the cause?"

The Bigger Picture: Costs, Trends, and Hope
Preventable drug reactions in older adults cost the U.S. $30 billion a year. That’s 15% of all medication spending for seniors. Hospitals are now penalized for high readmission rates tied to medication errors-so change is coming. New tools are helping. AI systems like MedAware reduce medication errors by 42%. Pharmacogenomic testing (checking your genes for how you metabolize drugs) cuts adverse reactions by 35% in seniors on psychiatric meds. The FDA now encourages including older adults in clinical trials. By 2026, they want 25% of trial participants to be over 75. That’s a big step. And the deprescribing movement is growing. Doctors are learning it’s not always better to add more drugs. Sometimes, the best treatment is to stop one.Bottom Line: It’s Not About Age-It’s About Adaptation
Aging doesn’t mean you can’t take medicine safely. It means you need smarter prescribing. The same pill, same dose, same routine-it’s not the same for your body at 80 as it was at 50. If you or a loved one is over 65 and on multiple medications, don’t assume everything is fine. Side effects aren’t "just part of getting older." They’re warning signs. Ask questions. Demand reviews. Push for adjustments. The goal isn’t to stop all meds. It’s to make sure every one still earns its place in your life.Why do older adults have more side effects from medications?
Older adults have more side effects because aging changes how the body absorbs, processes, and responds to drugs. Kidney and liver function decline, body composition shifts (less water, more fat), and brain sensitivity to certain drugs increases. Even at the same dose, drugs can build up to toxic levels or cause stronger reactions than in younger people.
What are the most dangerous medications for seniors?
The Beers Criteria lists the riskiest drugs for older adults, including anticholinergics like Benadryl (cause confusion), benzodiazepines like Xanax (increase fall risk), NSAIDs like ibuprofen (cause kidney and stomach damage), and certain antidepressants like amitriptyline (trigger urinary retention). Many of these are still commonly prescribed despite safer alternatives.
How can I tell if a medication is causing problems in an older adult?
Watch for new or worsening symptoms like dizziness, confusion, memory lapses, falls, constipation, unexplained weight loss, or urinary problems. These aren’t normal aging signs-they’re often red flags for medication side effects. If symptoms started after a new drug was added, that’s a strong clue.
Should seniors always take lower doses of medication?
Yes, for most medications, especially those cleared by the kidneys or liver. Starting at 25-50% of the standard adult dose and increasing slowly is the safest approach. But not all drugs need lower doses-some work the same. The key is individualized dosing based on kidney function, weight, and overall health-not just age.
What is deprescribing, and why is it important?
Deprescribing means stopping medications that are no longer needed or that pose more risk than benefit. It’s important because many older adults take drugs prescribed years ago for conditions that have changed or resolved. Stopping unnecessary meds reduces side effects, lowers fall risk, improves quality of life, and can even extend independence.
 Nov, 19 2025
Nov, 19 2025
swatantra kumar
November 20, 2025 AT 04:36robert cardy solano
November 21, 2025 AT 16:47Lemmy Coco
November 23, 2025 AT 08:30serge jane
November 25, 2025 AT 02:18Cinkoon Marketing
November 25, 2025 AT 14:26Pawan Jamwal
November 26, 2025 AT 09:10rob lafata
November 27, 2025 AT 10:04Matthew McCraney
November 27, 2025 AT 15:12Bill Camp
November 28, 2025 AT 20:33