MAOI Drug Interaction Checker
Check if your medication is safe
Enter any medication name to see if it's dangerous when combined with MAOI antidepressants like Nardil or Parnate.
One pill. That’s all it takes. A cold medicine you picked up at the store. A supplement you thought was harmless. And if you’re on an MAOI antidepressant, that one pill can trigger a blood pressure spike so violent it bursts blood vessels in your brain. This isn’t science fiction. It’s a documented, preventable death sentence - and it happens more often than you think.
What Happens When Ephedrine Meets an MAOI
Ephedrine is a stimulant. It’s in some cold and asthma meds, weight loss pills, and energy supplements. It works by forcing your body to release norepinephrine - the same chemical your brain uses to ramp up heart rate, tighten blood vessels, and raise blood pressure. On its own, it’s risky for people with heart conditions. But when it meets an MAOI, it becomes a bomb. MAOIs - monoamine oxidase inhibitors - are antidepressants like phenelzine (Nardil), tranylcypromine (Parnate), and isocarboxazid (Marplan). They work by blocking an enzyme called monoamine oxidase. That enzyme normally breaks down excess norepinephrine, serotonin, and dopamine. Without it, those chemicals pile up. Normally, that’s good for depression. But when ephedrine floods your system with even more norepinephrine, your body has no way to clean it up. The result? A hypertensive crisis. Blood pressure can jump from normal to over 200 mmHg systolic in under an hour. That’s like a garden hose connected to a fire hydrant. Your arteries can’t handle it. Blood vessels rupture. Strokes happen. Heart attacks follow. Subarachnoid hemorrhages - bleeding in the space around the brain - have been reported after just one 25 mg dose of ephedrine in patients on MAOIs.The Real-World Cases: It’s Not Theoretical
In 1965, a 49-year-old woman took a single dose of ephedrine while on nialamide, an MAOI. Within 30 minutes, she collapsed. A CT scan showed bleeding in her brain. She died. That case was published in JAMA - one of the first warnings. Fast forward to 2018. A 32-year-old man took a 25 mg ephedrine tablet for congestion. He was on phenelzine. His blood pressure hit 240 mmHg. He suffered a brain hemorrhage. He survived, but barely. Reddit threads from 2020 to 2023 are full of similar stories. Users write about “explosive headaches,” “vision going white,” and “feeling like my head would burst.” One user, u/MAOIsurvivor, wrote: “I thought it was just a bad migraine. By the time I got to the ER, my BP was 230/130. I spent three days in the ICU.” The FDA’s own database recorded 37 cases of hypertensive crisis from MAOI-ephedrine interactions between 2015 and 2020. Nine of them were fatal.It’s Not Just Ephedrine - It’s the Whole Class
You might think, “I don’t take ephedrine.” But ephedrine isn’t the only problem. Pseudoephedrine - the active ingredient in Sudafed - acts the same way. So does phenylephrine, found in many “non-drowsy” cold remedies. Even phenylpropanolamine, banned in the U.S. but still sold overseas, carries the same risk. These aren’t rare ingredients. They’re in over-the-counter nasal sprays, cough syrups, and energy shots. A single 12.5 mg dose of pseudoephedrine - half a tablet - can trigger a crisis in someone on an MAOI. That’s less than what’s in a typical decongestant. And it’s not just oral meds. Some topical nasal sprays contain these stimulants. Even some weight-loss patches and dietary supplements list “natural stimulants” without naming ephedrine or pseudoephedrine outright. If it says “stimulant,” “decongestant,” or “sympathomimetic,” assume it’s dangerous.
How Long Does the Danger Last?
Here’s where people get tripped up. You think, “I stopped my MAOI last week. I’m safe now.” You’re not. Irreversible MAOIs like Nardil and Parnate permanently disable the monoamine oxidase enzyme. Your body has to grow new enzymes to replace them. That takes 2 to 3 weeks. Even after you stop taking the drug, your system is still vulnerable. The FDA, the American Psychiatric Association, and StatPearls all agree: you must wait at least 14 days after stopping an irreversible MAOI before taking any sympathomimetic. For some doctors, they recommend 21 days just to be safe. Reversible MAOIs like moclobemide are less dangerous. The enzyme inhibition only lasts 24 to 48 hours. But even then, you still need to avoid ephedrine and pseudoephedrine. There’s no safe gray area.What Happens in the ER? It’s Not What You Think
If someone ends up in the emergency room with a hypertensive crisis from this interaction, time is everything. The goal isn’t just to lower blood pressure - it’s to lower it safely. You might assume, “Just give them a blood pressure pill.” But that’s deadly wrong. Sublingual nifedipine, a common quick-acting drug, can cause a sudden, uncontrolled drop in pressure. That can trigger a stroke. It’s banned in this scenario. The only safe option is intravenous phentolamine. It’s a fast-acting alpha-blocker that directly counters the norepinephrine surge. It’s given slowly, under constant monitoring. The dose? 5 to 15 mg, titrated by response. This isn’t something you can do at home. It requires ICU-level care.Why Do People Still Get This Wrong?
MAOIs are prescribed to less than 1% of depressed patients today. But they’re still vital for treatment-resistant depression - especially atypical depression with mood reactivity, excessive sleep, and increased appetite. About 500,000 Americans are on them right now. The problem? Most primary care doctors don’t know the risks. A 2021 study in JAMA Internal Medicine found that 22% of patients prescribed MAOIs were still given at least one contraindicated medication within 30 days - often by a non-psychiatrist. Patients don’t always know what they’re taking. They buy cold medicine without reading labels. They don’t tell their pharmacist they’re on an MAOI. They assume “natural” means safe.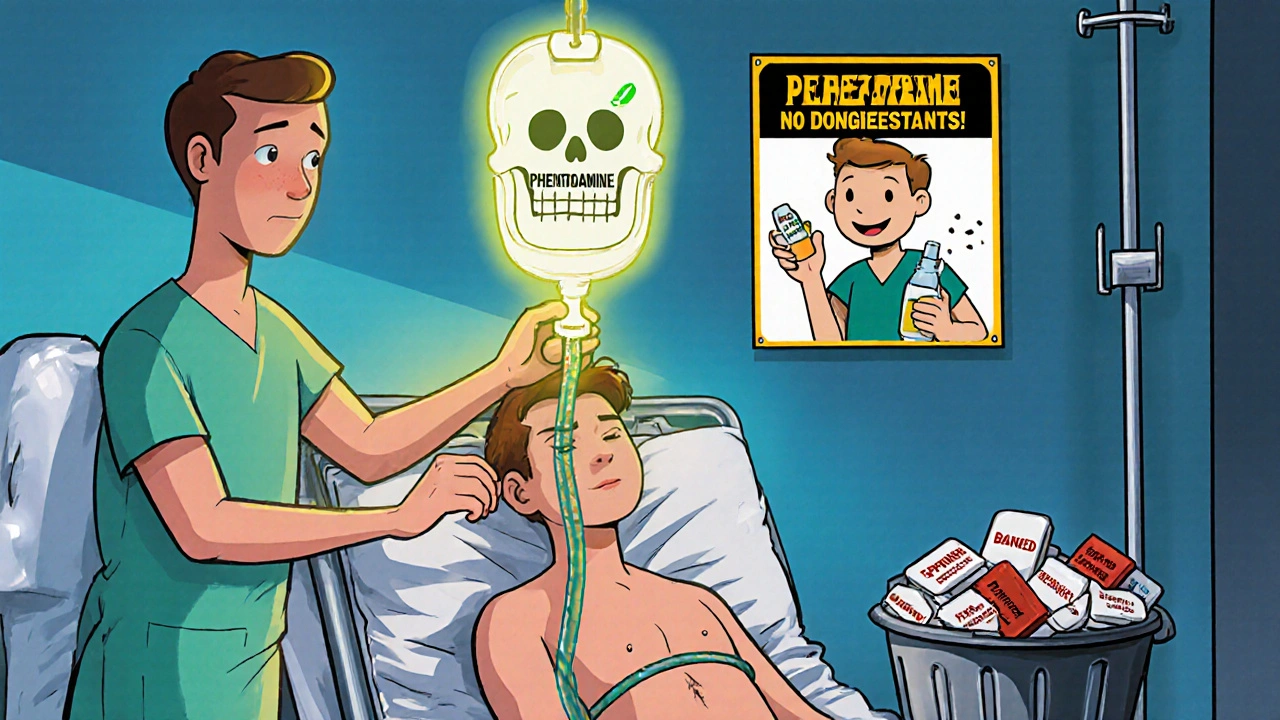
How to Stay Safe
If you’re on an MAOI, here’s your survival checklist:- Avoid all decongestants: No pseudoephedrine, phenylephrine, ephedrine, or phenylpropanolamine. Check every OTC label - even “herbal” ones.
- Wait 14 to 21 days after stopping: Don’t rush. Your body needs time to rebuild enzymes.
- Carry an MAOI alert card: The Mayo Clinic found that 87% of patients who carried these cards avoided dangerous interactions. Print one. Keep it in your wallet.
- Tell every doctor and pharmacist: Even your dentist. Even your eye doctor. Say: “I’m on an MAOI. I cannot take any stimulants or decongestants.”
- Use alternatives: For congestion, try saline nasal spray, steam inhalation, or antihistamines like loratadine (Claritin) - which are safe with MAOIs.
The Future: Are MAOIs Becoming Obsolete?
Some experts say yes. Dr. David Healy argues MAOIs should be pulled from the market because of the risk. Between 2000 and 2020, 127 people died from MAOI-drug interactions. But others say no. Dr. Charles Nemeroff calls them “the most effective antidepressants for certain types of depression.” And the FDA approved a new reversible MAOI, befloxatone, in March 2023 - with a 90% lower risk of hypertensive crisis. NIH is also testing wearable BP monitors that could warn users of early spikes. But until those are widely available, the rule stays the same: never combine ephedrine or any decongestant with an MAOI.Final Warning
This isn’t about being careful. This is about survival. One mistake. One unlabeled pill. One moment of forgetfulness. And it’s over. If you’re on an MAOI, treat every cold medicine like a loaded gun. If you’re not on one, but someone you care about is - make sure they know. Print the list. Put it on the fridge. Tell them to carry the card. This interaction kills. It doesn’t just raise blood pressure. It shatters lives. And it’s 100% preventable.Can I take Sudafed if I’m on an MAOI?
No. Sudafed contains pseudoephedrine, which acts exactly like ephedrine in the body. It triggers norepinephrine release. If you’re on an MAOI, taking Sudafed can cause a life-threatening hypertensive crisis. Even one tablet can be dangerous. Use saline sprays or antihistamines like Claritin instead.
How long after stopping an MAOI is it safe to take ephedrine?
Wait at least 14 days after stopping irreversible MAOIs like Nardil or Parnate. Many doctors recommend 21 days because it takes that long for your body to produce new monoamine oxidase enzymes. For reversible MAOIs like moclobemide, 24 to 48 hours is usually enough. But never guess - always check with your prescriber.
Are all MAOIs equally dangerous with ephedrine?
All MAOIs carry this risk, but the danger level varies. Irreversible MAOIs like phenelzine and tranylcypromine are the most dangerous because they permanently disable the enzyme. Reversible ones like moclobemide and the newer befloxatone have lower risk, but still require caution. Even low-dose transdermal selegiline (Emsam) can cause a crisis if combined with ephedrine. Never assume one is safe.
What should I do if I accidentally take ephedrine while on an MAOI?
Call 911 or go to the nearest ER immediately. Do not wait for symptoms. High blood pressure can spike within 30 minutes. Symptoms include severe headache, chest pain, blurred vision, nausea, or a feeling that your head will explode. Tell them you’re on an MAOI and took a decongestant. Do not take any blood pressure pills yourself - especially nifedipine. Only IV phentolamine is safe in this situation.
Can I use herbal supplements like ephedra if I’m on an MAOI?
No. Ephedra is a natural source of ephedrine. Even though it’s labeled “herbal” or “natural,” it contains the same active compound and carries the same deadly risk. The FDA banned ephedra in 2004 for weight loss products, but some supplements still sneak it in under other names. If it says “ma huang,” “ephedra,” or “stimulant blend,” avoid it completely.
Is there a safe decongestant for people on MAOIs?
Yes - but only a few. Saline nasal sprays, steam inhalation, and humidifiers are completely safe. Antihistamines like loratadine (Claritin), cetirizine (Zyrtec), or fexofenadine (Allegra) are also safe because they don’t affect norepinephrine. Avoid anything labeled “decongestant,” “stimulant,” or “sinus relief.” Always double-check with your pharmacist before taking anything new.
 Oct, 8 2025
Oct, 8 2025

Patrick Merk
November 16, 2025 AT 06:48Man, I never realized how many everyday meds could be landmines. I took Sudafed last winter thinking it was just a cold pill-thank god I wasn’t on an MAOI. This post is a wake-up call. I’m printing out that checklist and taping it to my fridge. Seriously, someone needs to make this a public service announcement.
Liam Dunne
November 17, 2025 AT 08:24Had a friend on phenelzine who almost died from a decongestant. She didn’t even know she was at risk. Pharmacists don’t always flag it either. This needs to be on every Rx bottle. Not just a footnote. Like, bold red letters: ‘DO NOT MIX WITH COLD MEDS.’
Phil Best
November 18, 2025 AT 03:19So let me get this straight. You can take a pill that says ‘natural energy booster’ from some guy in a van at a music festival, but if you’re on an MAOI, even a single Sudafed tablet turns you into a human bomb? And the FDA only logged 37 cases? Bro. That’s like saying ‘only 37 people died from jumping off the Golden Gate Bridge’-the real number’s way higher because most just… disappear.
Parv Trivedi
November 18, 2025 AT 07:53This is an extremely important health alert. Many people in developing countries are unaware of drug interactions, especially when using over-the-counter medications. I recommend that healthcare providers in all regions distribute printed materials in local languages. Awareness saves lives.
Willie Randle
November 19, 2025 AT 15:03One of the most terrifying things about this is how easily it’s avoidable. You don’t need a PhD to read a label. You don’t need a medical degree to say, ‘I’m on an MAOI, what’s safe?’ But people skip steps because they’re tired, or rushed, or think ‘it’s just one pill.’ One pill. One moment of carelessness. One irreversible mistake. This isn’t just medical advice-it’s a survival manual.
Connor Moizer
November 20, 2025 AT 19:27Stop being passive. If you’re on an MAOI, you don’t get to be lazy. You don’t get to assume ‘natural’ means safe. You don’t get to trust a random pharmacist who’s on their 12th shift. You carry the card. You call your doctor. You Google every ingredient. This isn’t a suggestion. It’s a damn lifeline. And if you’re not willing to treat it that way, you’re playing Russian roulette with your brain.
kanishetti anusha
November 21, 2025 AT 02:43I’ve been on moclobemide for two years and never knew the risks with pseudoephedrine. I thought only the old-school MAOIs were dangerous. This changed everything. I just threw out my entire medicine cabinet. Now I only use saline sprays. Thank you for writing this. I’ll share it with my support group.
roy bradfield
November 22, 2025 AT 10:43Let’s be real-this whole MAOI thing is a pharmaceutical scam. The FDA knew about these interactions for decades. Why didn’t they ban MAOIs outright? Why are they still sold? Because the drug companies make more money keeping people on lifelong meds than curing depression with therapy or lifestyle changes. And now they’re pushing ‘safer’ versions like befloxatone? That’s just the next product line. They don’t care if you die-they care about your subscription fee.
Sharon Campbell
November 24, 2025 AT 09:49ehhh idk i think this is overblown. i took pseudoephedrine once and felt fine. maybe its just fearmongering? also why do people even take MAOIs? they sound like a pain in the ass.
sara styles
November 25, 2025 AT 04:36Of course they’re pushing ‘reversible’ MAOIs. They’ve been testing this for years. The real danger isn’t the drug interaction-it’s the fact that MAOIs are being used as a Trojan horse to normalize long-term psychiatric dependency. The FDA’s 37 reported cases? That’s the tip of the iceberg. The real numbers are hidden in death certificates labeled ‘hypertensive stroke’ or ‘sudden cardiac arrest.’ They don’t want you connecting the dots. But now you know. And once you know, you can’t un-know it.
Brendan Peterson
November 25, 2025 AT 14:56Just to clarify: the 14-day rule applies to irreversible MAOIs. For reversible ones like moclobemide, the window is much shorter. But the key is consistency. If you’re going to be on an MAOI, you need to treat every OTC med like a potential threat. It’s not paranoia-it’s protocol. And if your doctor doesn’t know this, find a new one.
Jessica M
November 25, 2025 AT 17:27As a pharmacist with over 15 years of experience, I can confirm that this interaction is one of the most under-recognized causes of preventable death in psychiatric care. I have personally counseled over 200 patients on MAOIs. I provide printed handouts, follow-up calls, and even barcode scans at checkout to flag contraindicated products. This is not theoretical. It is clinical reality. Please, if you are on an MAOI-do not rely on memory. Do not assume safety. Always ask. Always verify. Lives depend on it.