Medication Risk Assessment Tool
Assess your current medication profile for potential deprescribing opportunities. Based on evidence from JAMA Internal Medicine and deprescribing.org guidelines.
Select Your Current Medications
Your Deprescribing Assessment
Next Steps
Discuss these findings with your healthcare team. You can download free tools from deprescribing.org including STOPP/START criteria and Beers Criteria.
Every year, millions of older adults take more medications than they need. Some of these drugs were prescribed years ago for conditions that have since changed-or disappeared. But no one ever stopped them. The result? A growing pile of pills, each with its own risks, each adding to the chance of dizziness, falls, confusion, or hospital visits. This isn’t laziness. It’s a system designed to start treatments, not stop them. That’s where deprescribing comes in.
What Deprescribing Really Means
Deprescribing isn’t just stopping pills. It’s not cutting corners or ignoring doctors’ orders. It’s a careful, step-by-step process of reviewing every medication a person takes and asking: Is this still helping? Or is it hurting more than it helps? The goal is simple: reduce harm, not just pills. The term became official around 2012, thanks to researchers in Canada who saw how often older adults were stuck on drugs that no longer made sense. One of those researchers, Dr. Cara Tannenbaum, helped build the first real framework for doing this safely. Today, deprescribing.org is the go-to resource for clinicians worldwide. And the data shows it works. A 2023 study in JAMA Internal Medicine followed 372 older adults in post-acute care. Those who went through a structured deprescribing process ended up taking 1.8 fewer medications on average. And here’s the surprise: their risk of falls, confusion, or hospital stays didn’t go up. It stayed the same. That means you can cut back-and stay just as safe, if not safer.Which Medications Are Most Often Stopped
Not all drugs are created equal when it comes to deprescribing. Some are high-risk, low-reward. Five classes stand out as the most common targets:- Proton-pump inhibitors (PPIs) - These are heartburn drugs like omeprazole. Many people take them for years, even though they were only meant for short-term use. Long-term use raises the risk of bone fractures, kidney problems, and infections.
- Benzodiazepines and sleep aids - Drugs like diazepam or zolpidem. These increase fall risk by 50% in people over 65. They also cause memory fog and can lead to dependence.
- Antipsychotics - Often prescribed for dementia-related agitation, even though they’re not approved for that use. These drugs can cause tremors, stiffness, and even sudden death in older adults.
- Antihyperglycemics - Diabetes medications like sulfonylureas. In frail older adults, low blood sugar can be deadly. Tight control isn’t always better.
- Opioid painkillers - Long-term use for chronic pain rarely improves function. But it increases the risk of addiction, constipation, and respiratory depression.
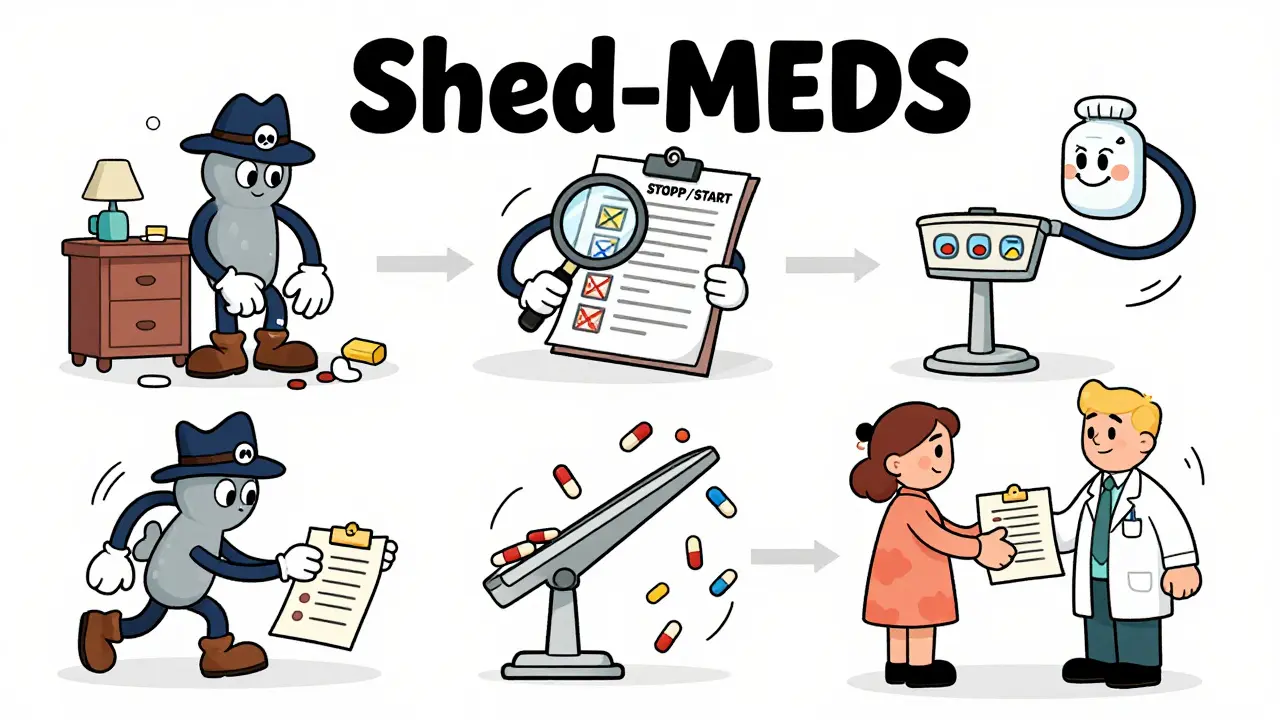
The Shed-MEDS Framework: How It Works
One of the most validated tools is called Shed-MEDS. It’s a four-step process used in hospitals and clinics across North America:- Best Possible Medication History - Get the full list. Not what the patient remembers. Not what the chart says. What they’re actually taking, including over-the-counter pills and supplements.
- Evaluate - Use tools like STOPP/START criteria or the Beers Criteria to flag drugs that are inappropriate for age or condition.
- Deprescribing Recommendations - Prioritize which drugs to stop first. Start with the ones with the highest risk and lowest benefit.
- Synthesis - Talk to the patient. Explain why you’re suggesting a change. Get their input. Build a plan together.
Why Most Clinicians Struggle to Do It
You’d think with all this evidence, deprescribing would be routine. But it’s not. A 2022 study in the Canadian Medical Association Journal found fewer than 15% of primary care doctors regularly use deprescribing frameworks. Why? Time. The average visit lasts 7.2 minutes. That’s not enough to review 10 medications, check for interactions, explain risks, and answer fears. Another problem? EHRs. Most electronic health records are built to remind doctors to add medications. They rarely prompt: “Have you considered stopping this?” And then there’s fear. Patients have been on these pills for 10, 15, even 20 years. They believe the pill is keeping them alive. Stopping it feels like giving up. One 2022 study found 22% of older adults felt anxious about stopping even a single medication. Pharmacists, on the other hand, are leading the charge. When pharmacists are part of the team, deprescribing success rates jump 35-40%. Why? They’re trained in medication therapy management. They have the time. They’re not rushing between patients.What Happens When You Don’t Deprescribe
The cost of doing nothing is staggering. The World Health Organization reports that 40% of older adults globally are on five or more medications - a condition called polypharmacy. In the U.S., medication-related problems cause 30% of hospital admissions in people over 65. Many of those admissions are preventable. A 2024 analysis of 80 clinical guidelines found that only 7% included any deprescribing advice. Meanwhile, 93% focused on when to start a drug. That imbalance is dangerous. We’ve spent decades teaching doctors how to prescribe. We’ve barely started teaching them how to stop. And it’s not just hospitals. It’s families. It’s caregivers. It’s the elderly woman who takes 12 pills a day and can’t remember which ones are for her blood pressure, which for sleep, which for pain she doesn’t even feel anymore.
How to Start Deprescribing - Even If You’re Not a Doctor
You don’t need to be a specialist to help. If you’re caring for an older adult, here’s what you can do:- Make a complete list - Write down every pill, patch, cream, vitamin, and supplement. Include doses and how often they’re taken. Bring this to every appointment.
- Ask the big question - “Why was this prescribed? Is it still needed?” Don’t be afraid to ask twice.
- Look for red flags - Dizziness, confusion, falls, constipation, extreme fatigue. These aren’t just “part of aging.” They might be side effects.
- Use free tools - Go to deprescribing.org. Download the STOPP/START criteria or the Beers Criteria. They’re free, updated yearly, and designed for non-experts.
- Push for pharmacist involvement - Ask if your clinic has a medication therapy management program. If not, request one.
The Future Is Here - But It’s Not Everywhere
Change is coming. The American Medical Association passed its first deprescribing policy in June 2024, saying doctors must regularly assess whether all medications are still appropriate. The Centers for Medicare & Medicaid Services will start tying payments to deprescribing performance in 2026. In Canada, the DIGE program has been nationally adopted since 2018. In the U.S., only 28% of primary care practices have formal deprescribing protocols. That gap is closing - slowly. AI tools are being developed to scan EHRs and flag potential deprescribing candidates. The NIH has invested $8.7 million since 2020 to expand guidelines to cover antidepressants, anticoagulants, and other high-risk classes. By 2030, experts predict deprescribing assessments will be as routine as checking blood pressure. But until then, progress depends on patients, families, and frontline clinicians speaking up.What to Do Next
If you’re a patient or caregiver: gather your medication list. Pick one drug you’re unsure about. Ask your doctor: “Could this be stopped?” If you’re a clinician: start with one class - PPIs or sleep aids. Use deprescribing.org’s free algorithms. Involve your pharmacist. Track your results. If you’re a health system leader: build deprescribing into your EHR. Train your staff. Reward it. This isn’t about taking away care. It’s about restoring it. Fewer pills. Fewer side effects. More clarity. More life.Is deprescribing the same as stopping medications cold turkey?
No. Deprescribing is never about sudden stops. It’s a planned, gradual reduction based on evidence and patient response. For example, benzodiazepines are tapered over weeks to avoid seizures or rebound anxiety. PPIs are lowered slowly to prevent acid rebound. Each step is monitored, and adjustments are made based on symptoms.
Can deprescribing cause harm?
When done properly, deprescribing reduces harm. Studies show no increase in hospitalizations, falls, or deaths - even when patients stop multiple medications. The real danger is continuing drugs that no longer help. A 2023 trial found no difference in adverse events between patients who deprescribed and those who didn’t - despite a significant drop in pill count.
Who should consider deprescribing?
Anyone taking five or more medications, especially older adults with multiple chronic conditions. But it’s not just about age. Frailty, life expectancy, and personal goals matter more. Someone with advanced dementia may not need a statin. Someone with limited mobility may not need a diabetes drug that causes low blood sugar. Deprescribing is personalized.
Why aren’t more doctors doing this?
Time, training, and tools. Most doctors get little education on stopping meds. EHRs don’t prompt them to review existing prescriptions. Visits are too short. And there’s fear - of patient pushback, of missing something, of being blamed if symptoms return. But the biggest barrier? We’ve never been taught how to stop - only how to start.
Are there free tools I can use?
Yes. Deprescribing.org offers free, evidence-based guidelines for PPIs, benzodiazepines, antipsychotics, antihyperglycemics, and opioids. The Beers Criteria and STOPP/START version 3 are also publicly available. These are used by hospitals and clinics worldwide. You don’t need a subscription - just access.
How long does it take to see results after stopping a medication?
It varies. For sleep aids like zolpidem, improvement in balance and alertness can happen within days. For PPIs, reflux may return in 2-4 weeks, signaling the need to adjust the taper. For antipsychotics, agitation may take weeks to improve as the brain readjusts. Monitoring is key - symptoms should be tracked weekly during the taper.
 Dec, 15 2025
Dec, 15 2025
Aditya Kumar
December 16, 2025 AT 01:27Yeah sure, sounds great in theory. But who’s actually gonna do the work? Doctors are burnt out, patients are scared, and the system doesn’t care unless it’s billing for another script.
James Rayner
December 16, 2025 AT 23:03I’ve watched my dad take 14 pills a day… for 12 years. Half of them were for things he doesn’t even have anymore. When we finally asked his doctor to review them? He cried. Not from sadness-because he felt seen. We cut 5. His balance improved. His mind cleared. It wasn’t magic. It was just… attention.
Josias Ariel Mahlangu
December 17, 2025 AT 20:36This is just another way for Big Pharma to offload responsibility. They profit from pills. They don’t want you stopping them. The ‘evidence’? Paid for by the same labs that make the drugs. Wake up.
Dave Alponvyr
December 18, 2025 AT 11:21So… you’re telling me we’ve spent 50 years teaching doctors to prescribe… but not to stop? 🤦♂️
Cassandra Collins
December 20, 2025 AT 07:09Deprescribing? That’s what they call it now. But I know the truth-this is all part of the government’s plan to kill off old people with ‘natural causes’ so they don’t have to pay Social Security. They’re already putting toxins in the water to make us forget our meds. You think this is about safety? It’s about control.
Joanna Ebizie
December 22, 2025 AT 03:06OMG I’m so tired of people who think taking 10 pills a day is normal. You’re not ‘managing health’-you’re just medicating away your problems. My grandma stopped her statin and now she walks 3 miles a day. No doctor told her to. She just did it. Why can’t everyone be that brave?
Elizabeth Bauman
December 23, 2025 AT 15:54Let me get this straight-some Canadian researchers came up with a framework, and now we’re supposed to trust it? In America, we don’t follow foreign medical trends just because they sound nice. We’ve got our own system. And if your grandma’s on a pill that’s been working for 20 years, leave it alone. This is cultural erosion disguised as ‘evidence.’
Dylan Smith
December 24, 2025 AT 07:19I love that this exists but why is it still so hard to get pharmacists involved? My mom’s pharmacist caught three unnecessary meds last month. Why aren’t we funding these people more? Why are they stuck in the back while doctors rush through 20 patients an hour? This isn’t about pills-it’s about who we value in healthcare
Mike Smith
December 25, 2025 AT 13:18Thank you for sharing this. This is not just clinical-it’s human. Deprescribing is dignity. It’s autonomy. It’s saying, ‘Your life matters more than your prescription list.’ The systems are broken, but the principles are clear: listen, review, reduce, repeat. And if you’re reading this-start with one pill. Ask one question. That’s how change begins.
Ron Williams
December 26, 2025 AT 11:37My cousin in India takes 8 meds. She’s 72. Never been to a doctor in 15 years. Just gets refills from the local shop. This whole framework? It’s beautiful. But it’s for people who have access. What about the 80% of the world who don’t? We need global tools. Not just American guidelines.