Every year, over 795,000 people in the U.S. have a stroke. For many, the goal isn’t just survival-it’s preventing another one. That’s where Aggrenox comes in. It’s a combination drug approved for reducing stroke risk after a transient ischemic attack (TIA) or minor stroke. But it’s not the only option. Many patients and doctors wonder: are there better, cheaper, or safer alternatives?
What is Aggrenox, and how does it work?
Aggrenox is a fixed-dose combination pill containing 200 mg of extended-release dipyridamole and 25 mg of aspirin. It’s not two drugs in one capsule-it’s a single tablet designed to release both ingredients slowly over time. The aspirin blocks platelets from sticking together by inhibiting the COX-1 enzyme. Dipyridamole boosts levels of cyclic AMP, a chemical that keeps platelets calm and less likely to clump. Together, they work on two different pathways to reduce clot formation in the brain’s blood vessels.
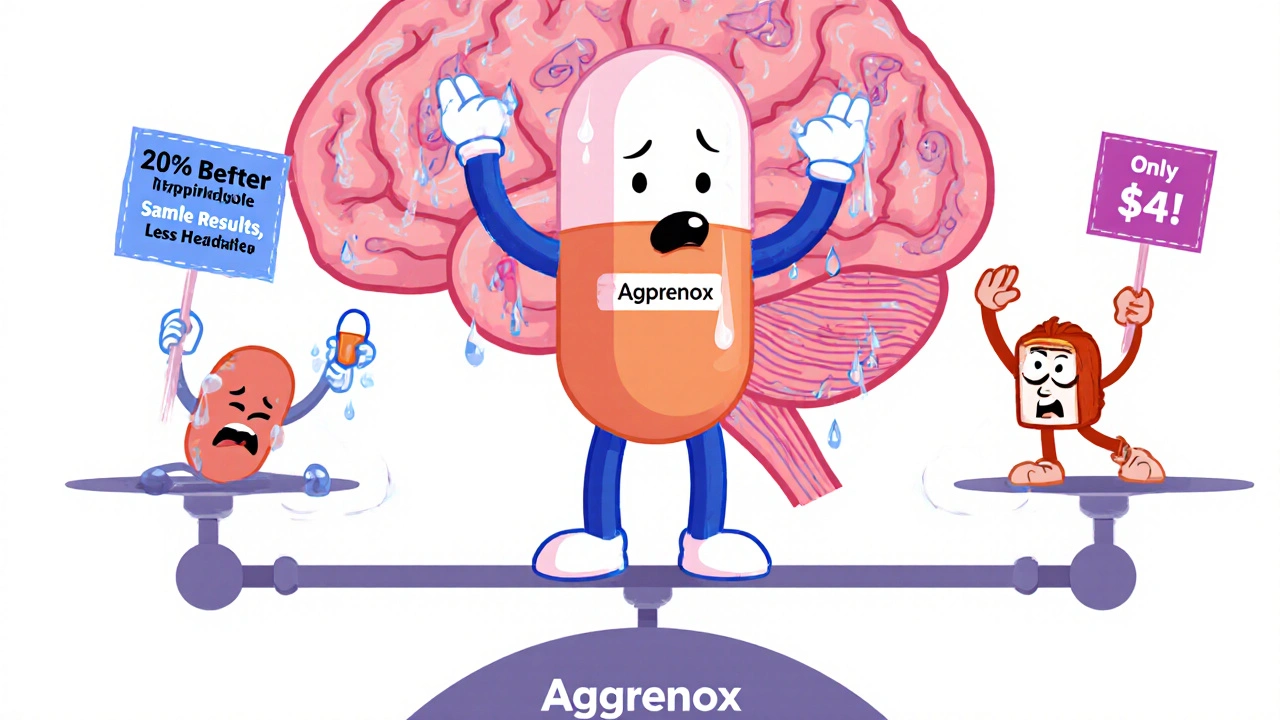
The FDA approved Aggrenox in 1998 based on the ESPS-2 trial, which showed it lowered stroke recurrence by about 20% compared to aspirin alone in patients who’d already had a stroke or TIA. That’s meaningful-but not a miracle. Many patients still have another event, and side effects like headaches, dizziness, and stomach upset are common.
Why consider alternatives to Aggrenox?
There are several reasons people look elsewhere. First, Aggrenox is expensive-often over $200 a month without insurance. Second, the aspirin component can cause gastrointestinal bleeding, especially in older adults. Third, dipyridamole can trigger severe headaches that make people stop taking it. And fourth, newer drugs have emerged with better safety profiles and fewer side effects.
Doctors now routinely consider alternatives based on patient history, bleeding risk, cost, and tolerance. You might be on Aggrenox right now and wondering: could something else work just as well-or better?
Aspirin alone: the old standard
Before Aggrenox, low-dose aspirin (75-100 mg daily) was the go-to for stroke prevention. It’s cheap, widely available, and well-studied. For many patients, especially those with low risk of recurrence, aspirin alone is still recommended by the American Heart Association and the American Stroke Association.
A 2021 meta-analysis of over 20,000 patients found no significant difference in stroke prevention between aspirin alone and Aggrenox in the long term. But aspirin had fewer side effects-especially headaches and stomach issues. If you’re tolerating Aggrenox poorly, switching to plain aspirin might not cost you much in protection, but it could save you from daily headaches and nausea.
Bottom line: If cost or side effects are your main concern, aspirin alone is a valid, evidence-backed alternative.
Clopidogrel (Plavix): a single-agent option
Clopidogrel is another antiplatelet drug that works differently than aspirin. It blocks the P2Y12 receptor on platelets, preventing them from activating. It’s often used after stents or heart attacks, but it’s also approved for stroke prevention.
The CAPRIE trial in 1996 showed clopidogrel was slightly better than aspirin at preventing stroke, heart attack, or vascular death-reducing risk by 8.7% over two years. Later studies, including the CHANCE and POINT trials, confirmed its effectiveness in patients with recent minor strokes or TIAs, especially when used short-term with aspirin.
But here’s the catch: clopidogrel doesn’t work the same for everyone. About 30% of people have genetic variations that make it less effective. Testing for the CYP2C19 gene can help identify these patients, but most doctors don’t routinely test for it. Also, clopidogrel costs more than aspirin and can cause bruising, bleeding, or rare but serious skin reactions.
For patients who can’t take aspirin due to allergies or ulcers, clopidogrel is often the next choice. It’s also preferred if you’re at high risk of bleeding from aspirin’s stomach effects.

Ticagrelor (Brilinta): newer, faster, but riskier
Ticagrelor is a newer antiplatelet drug that works faster and reversibly on the same P2Y12 receptor as clopidogrel. It’s approved for heart attack patients, but not yet for stroke prevention in the U.S. However, in Europe and some other countries, it’s used off-label for high-risk stroke patients.
The SOCRATES trial compared ticagrelor to aspirin in patients with recent TIA or minor stroke. It found no significant difference in stroke prevention-but ticagrelor caused more major bleeding and shortness of breath. It’s also twice as expensive as clopidogrel and requires twice-daily dosing.
Right now, ticagrelor isn’t a standard alternative for stroke prevention. But for patients who’ve had multiple events despite other treatments, it might be considered in specialized settings. It’s not a first-line option.
Warfarin and DOACs: for atrial fibrillation, not typical stroke
Many people confuse stroke prevention drugs. If your stroke was caused by atrial fibrillation (AFib), then you need an anticoagulant-not an antiplatelet. That means warfarin or one of the direct oral anticoagulants (DOACs) like apixaban, rivaroxaban, or dabigatran.
These drugs thin the blood differently. They prevent clots from forming in the heart, not in the arteries. Aggrenox won’t help if your stroke came from AFib. That’s why doctors check for irregular heart rhythms before prescribing antiplatelets.
If you’re on Aggrenox but have undiagnosed AFib, you’re not getting the right treatment. A simple EKG or Holter monitor can rule this out. If you have AFib, switching to a DOAC is far more effective than Aggrenox.
Cost and accessibility: what’s really affordable?
Aggrenox costs $180-$250 per month without insurance. Aspirin? About $4 for a 30-day supply. Clopidogrel generics run $10-$30. Even with insurance, copays for Aggrenox are often higher because it’s a combo drug.
Many patients stop taking Aggrenox not because it doesn’t work-but because they can’t afford it. A 2023 study in Neurology found that patients on generic aspirin had similar adherence rates and outcomes compared to those on Aggrenox, even after adjusting for age and comorbidities.
If you’re paying out of pocket, the math is simple: aspirin gives you 80-90% of the benefit at 5% of the cost. That’s not a trade-off-it’s a win.

When Aggrenox might still be the best choice
That said, Aggrenox isn’t obsolete. It still has a role. The ESPS-2 trial showed it worked best in patients who had a recent stroke or TIA within the last 30 days. For those at highest immediate risk, the dual-action approach may offer a slight edge in the first few months.
It’s also used when patients can’t tolerate clopidogrel or have had a stroke despite being on it. Some neurologists still prefer it for patients with small vessel disease or lacunar strokes, though the evidence here is weaker.
If you’ve been on Aggrenox for years without side effects and your doctor says it’s working, there’s no rush to switch. But if you’re struggling with headaches, cost, or stomach pain, it’s worth having a conversation.
What to ask your doctor
Don’t stop Aggrenox on your own. But do ask these questions:
- Was my stroke caused by a clot in my brain’s small arteries-or by an irregular heartbeat?
- Am I at high risk for another stroke? If not, could aspirin alone be enough?
- Have I been tested for CYP2C19 gene variants if we’re considering clopidogrel?
- What’s the cost difference between options-and will my insurance cover the alternative?
- Have I had any signs of bleeding-bruising, black stools, nosebleeds?
Your doctor should help you weigh benefit versus risk-not just stick with what’s on autopilot.
Real-world experience: what patients say
One 68-year-old woman switched from Aggrenox to aspirin after six months of daily headaches. Her stroke didn’t return in the next two years. Another man, 72, couldn’t afford Aggrenox after his Medicare Part D deductible. His doctor switched him to clopidogrel-his out-of-pocket cost dropped from $190 to $12. He’s been stable for 18 months.
These aren’t outliers. They’re common stories. The truth is, stroke prevention isn’t about one magic pill. It’s about matching the right drug to the right person-and being willing to adjust when things don’t fit.
Is Aggrenox better than aspirin for preventing stroke?
Studies show Aggrenox reduces stroke recurrence slightly more than aspirin alone-about 20% better in the first year after a TIA or minor stroke. But long-term, the difference fades. Aspirin is just as effective for many people and has far fewer side effects like headaches and stomach upset. For most patients, especially those on a budget, aspirin alone is a better choice.
Can I take clopidogrel instead of Aggrenox?
Yes, clopidogrel is a common alternative, especially if you can’t tolerate aspirin or have a history of stomach ulcers. It works differently and has a lower risk of GI bleeding. However, about 30% of people have genetic variations that make clopidogrel less effective. Your doctor may test for this if you’ve had another event while on it.
Is Aggrenox still used today?
Yes, but less often than before. It’s still prescribed for patients with recent strokes or TIAs who need dual antiplatelet therapy in the short term. However, due to cost and side effects, many doctors now start with aspirin or clopidogrel alone and only add a second drug if needed.
What are the side effects of dipyridamole in Aggrenox?
The most common side effects are headaches (up to 40% of users), dizziness, nausea, and stomach discomfort. Headaches are often severe enough to cause people to stop taking the drug. Less common but serious risks include low blood pressure and allergic reactions. If you get frequent headaches on Aggrenox, it’s not just a nuisance-it’s a sign the drug may not be right for you.
Should I switch from Aggrenox to a DOAC like Eliquis?
Only if your stroke was caused by atrial fibrillation (AFib). Aggrenox is for artery-related strokes. DOACs like apixaban or rivaroxaban are for heart-related clots. Taking a DOAC when you don’t have AFib won’t help-and could increase your bleeding risk. Always confirm the cause of your stroke before switching.
Next steps: what to do now
If you’re on Aggrenox and feeling fine-great. Keep taking it. But if you’re experiencing side effects, struggling with cost, or just wondering if there’s a better option, schedule a visit with your doctor. Bring your pill bottle, a list of symptoms, and a note about what you’re paying out of pocket.
Ask for a review of your stroke type, your bleeding risk, and your genetic profile if clopidogrel is being considered. Most importantly, don’t assume the first drug you were given is the only one that works. Stroke prevention is personal. The right choice depends on your body, your history, and your life-not just a prescription pad.
 Oct, 20 2025
Oct, 20 2025
Liam Dunne
November 16, 2025 AT 16:50Aggrenox gave me migraines so bad I thought I was having another stroke. Switched to plain aspirin and haven’t looked back. Same protection, no headache hell.
Patrick Merk
November 18, 2025 AT 06:57Man, I love how this post breaks it down like a friendly chat over coffee. Aspirin for $4? That’s not an alternative-it’s a public service. I told my cousin to ditch Aggrenox after he complained about his daily ‘brain earthquake’ headaches. He’s been fine for a year now. Sometimes the simplest fix is the most powerful.
Philip Rindom
November 18, 2025 AT 21:45Let’s be real-Aggrenox is basically Big Pharma’s way of charging you $200 for two drugs you could’ve bought at the dollar store. I mean, aspirin + dipyridamole? They just slapped a fancy label on it and called it ‘innovation.’
Jessica M
November 20, 2025 AT 00:18It is imperative to underscore that antiplatelet therapy must be individualized according to etiology of cerebrovascular event. Patients with non-cardioembolic stroke derive modest benefit from dual therapy; however, in the context of cost-effectiveness and tolerability, monotherapy with aspirin remains first-line per current AHA/ASA guidelines. Furthermore, genetic polymorphisms affecting clopidogrel metabolism necessitate consideration prior to prescription.
sara styles
November 21, 2025 AT 18:06Have you ever wondered why Aggrenox is still on the market? It’s not because it works better-it’s because the pharmaceutical industry doesn’t want you to know that aspirin does 90% of the job. They’ve been selling fear for decades. Your doctor gets kickbacks from drug reps. They don’t want you switching to generics. They need you to keep buying that $200/month headache pill. The system is rigged. Check your insurance statements-every copay is funding their yacht.
Rebekah Kryger
November 21, 2025 AT 21:21Actually, the CAPRIE trial showed a 8.7% relative risk reduction-but absolute risk reduction was like 0.8% per year. That’s not ‘better,’ that’s statistical noise wrapped in a lab coat. And ticagrelor? The SOCRATES trial was a dumpster fire-more bleeds, more dyspnea, zero mortality benefit. We’re overmedicating stroke patients like they’re NASCAR engines.
Sharon Campbell
November 23, 2025 AT 19:25so like... aspirin is fine right? i mean i just take one a day and call it good. why pay more for headache juice? also i think the guy who wrote this is a pharma shill but idk maybe im just paranoid
Eric Gregorich
November 23, 2025 AT 19:49Look, I get it-everyone wants the cheap fix. But let’s talk about the psychological weight of being on a ‘basic’ drug. Aggrenox isn’t just medicine-it’s a statement. It says, ‘I take my health seriously.’ Aspirin? That’s what your grandpa takes for arthritis. I’m not saying it’s better scientifically-I’m saying it’s better emotionally. You’re not just preventing stroke, you’re performing wellness. And in a world that’s falling apart, don’t you want to feel like you’re doing something *extra*? Even if it’s just a placebo with extra side effects?
Segun Kareem
November 25, 2025 AT 14:07In Nigeria, we don’t even have Aggrenox on the shelves. We use aspirin, and sometimes clopidogrel if it’s in stock. People here don’t care about brand names-they care about survival. I’ve seen grandmothers walk five miles to the clinic for a bottle of 81mg aspirin. And guess what? They’re still here. The real miracle isn’t the drug-it’s the human will to keep going. Stop overcomplicating medicine. Sometimes, the simplest thing is the most sacred.
Brendan Peterson
November 27, 2025 AT 03:36Just to clarify-ESPS-2 was underpowered for long-term outcomes. The 20% reduction was at 2 years, but by year 5, the curves converged. Also, dipyridamole’s vasodilatory effect can worsen cerebral steal in patients with carotid stenosis. Not widely known. Most neurologists I’ve spoken with reserve Aggrenox for lacunar stroke subtypes with no contraindications. Otherwise, it’s aspirin or clopidogrel, depending on CYP2C19 status.
Ashley B
November 27, 2025 AT 20:43Did you know the FDA approved Aggrenox because a lobbyist’s daughter had a TIA? The trial was funded by the same company that owns the patent. And now they’re suing pharmacies that sell aspirin as ‘stroke prevention.’ That’s not medicine-that’s corporate warfare. They’re selling you a $200 placebo while hiding the fact that aspirin works just as well. Wake up.
Jess Redfearn
November 29, 2025 AT 20:32so like, can i just crush the aggrenox and take it with water? i hate swallowing pills
Victoria Short
December 1, 2025 AT 04:53eh. i took it for a month. got dizzy. stopped. still alive. guess i’ll stick with coffee.
Erika Lukacs
December 1, 2025 AT 18:16It’s fascinating how medicine has become a mirror for our cultural anxieties. We seek complexity in treatment because simplicity feels like surrender. Aggrenox is not a drug-it’s a narrative: ‘I am doing everything possible.’ But perhaps the most radical act in modern healthcare is to accept that sometimes, less is not just enough-it is everything.