If you’ve been prescribed Cipro (ciprofloxacin) and are wondering if there’s a better or safer option, you’re not alone. Many people ask the same thing - especially when they’ve heard about side effects, rising resistance, or cheaper generics. The truth is, Cipro isn’t always the best choice. It works well for some infections, but for others, there are safer, just as effective, or even more targeted alternatives. This guide breaks down exactly how Cipro stacks up against the most common antibiotics used today, so you know what to ask your doctor next time.
What is Cipro (ciprofloxacin) actually used for?
Ciprofloxacin, sold under the brand name Cipro, is a fluoroquinolone antibiotic. It fights bacteria by blocking enzymes they need to copy DNA and repair themselves. It’s not a broad-spectrum antibiotic like amoxicillin - it’s more focused. The FDA has approved it for specific infections:
- Urinary tract infections (UTIs), especially complicated ones
- Prostatitis (bacterial infection of the prostate)
- Respiratory infections like pneumonia in high-risk patients
- Skin and soft tissue infections
- Some types of gastrointestinal infections (like traveler’s diarrhea caused by E. coli)
- Anthrax exposure (post-exposure prophylaxis)
It’s not used for viral infections like colds or the flu. And it’s not first-line for simple UTIs or ear infections anymore - guidelines changed because of safety concerns.
Why doctors are moving away from Cipro
Back in the 1990s and early 2000s, Cipro was a go-to antibiotic. Today, it’s far less common - and for good reason. In 2016, the FDA issued a black box warning: fluoroquinolones like Cipro can cause serious, disabling side effects that may last for months or years. These include:
- Tendon rupture (especially the Achilles tendon)
- Nerve damage (peripheral neuropathy) - tingling, burning, numbness
- Central nervous system effects: anxiety, insomnia, hallucinations
- Low blood sugar (hypoglycemia), especially in diabetics
- Damage to aorta (increased risk of rupture)
A 2023 study in The BMJ found that patients taking fluoroquinolones had a 1.7 times higher risk of developing serious tendon issues within 90 days compared to those taking amoxicillin. That’s why the FDA now says these drugs should only be used when no other options exist - especially for mild infections like simple UTIs or sinus infections.
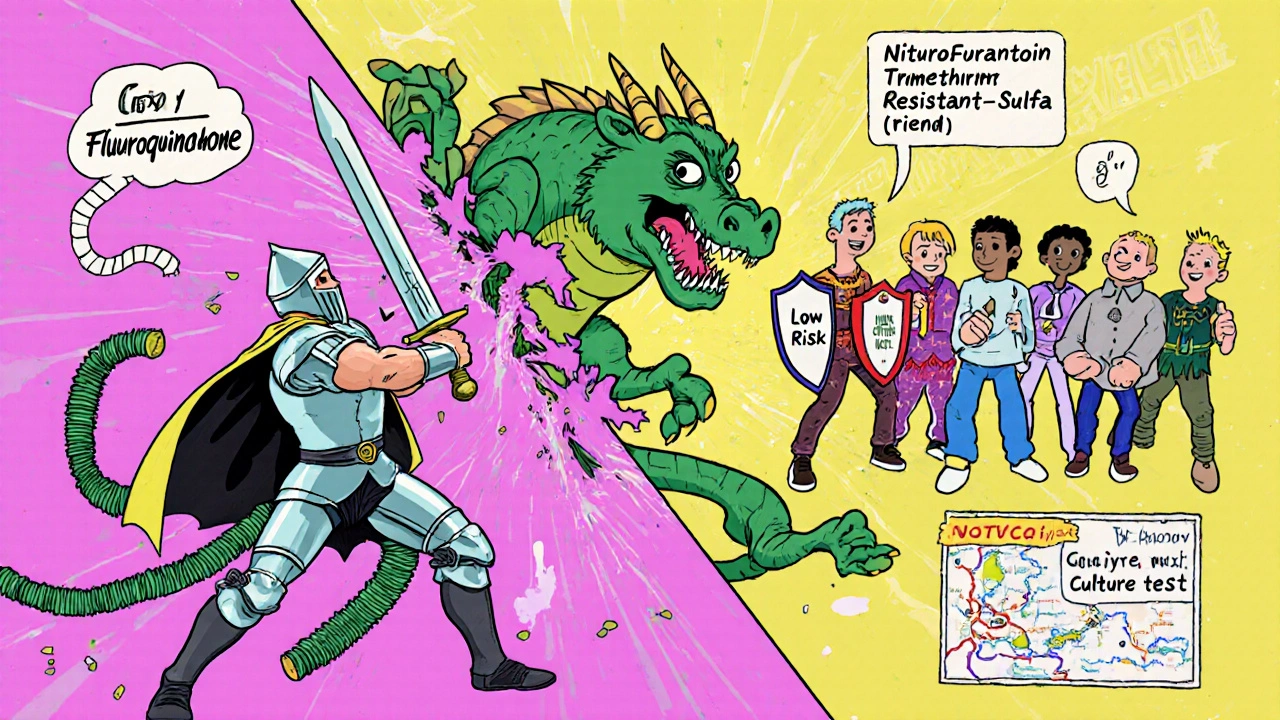
Top alternatives to Cipro and when to use them
Here are the most common antibiotics doctors now prescribe instead of Cipro - and why they’re better in most cases.
1. Nitrofurantoin - Best for simple UTIs
If you have an uncomplicated bladder infection (cystitis), nitrofurantoin is now the first choice. It’s taken orally, works directly in the urine, and rarely causes systemic side effects. It’s not absorbed into the bloodstream much, so it doesn’t affect tendons or nerves like Cipro does.
It’s not used for kidney infections (pyelonephritis) or prostate infections - it doesn’t reach those tissues well. But for 80% of UTIs, it’s just as effective and far safer.
2. Trimethoprim-sulfamethoxazole (Bactrim, Septra) - Good for UTIs and some respiratory infections
This combo drug has been around since the 1960s. It’s still effective against many strains of E. coli and other common UTI bugs. It’s also used for ear infections, bronchitis, and some skin infections.
Downside: People allergic to sulfa drugs can’t take it. Also, resistance is growing in some areas. But for most healthy adults, it’s a solid, low-cost alternative.
3. Fosfomycin (Monurol) - One-dose UTI treatment
For patients who want to avoid multi-day courses, fosfomycin is a single-dose powder you mix with water. It’s approved for uncomplicated UTIs and works quickly. It’s especially useful if you’ve had recurrent UTIs or are concerned about long-term antibiotic exposure.
It’s not used for kidney infections or in people with severe kidney disease, but for simple cases, it’s a game-changer.
4. Doxycycline - For respiratory, skin, and tick-borne infections
Doxycycline is a tetracycline antibiotic. It’s great for sinus infections, bronchitis, Lyme disease, acne, and some skin infections. It’s also used for pneumonia caused by atypical bacteria like Mycoplasma.
Unlike Cipro, it doesn’t carry tendon or nerve damage risks. It does cause sun sensitivity, so you need to avoid strong sunlight. And it shouldn’t be given to children under 8 or pregnant women.
5. Amoxicillin-clavulanate (Augmentin) - For sinus, ear, and lung infections
This is a penicillin-based combo drug. The clavulanate helps it fight bacteria that resist regular amoxicillin. It’s often used for sinus infections, ear infections, and pneumonia.
It’s safer than Cipro for most people, but if you’re allergic to penicillin, it’s off the table. Side effects include diarrhea and stomach upset - but rarely anything life-threatening.

Comparison table: Cipro vs top alternatives
| Antibiotic | Best For | Typical Duration | Key Side Effects | Cost (30-day generic) | Fluoroquinolone Risk? |
|---|---|---|---|---|---|
| Cipro (ciprofloxacin) | Complicated UTIs, prostatitis, anthrax | 7-14 days | Tendon rupture, nerve damage, low blood sugar | $20-$50 | Yes |
| Nitrofurantoin | Uncomplicated UTIs | 5-7 days | Stomach upset, rare lung issues (long-term use) | $10-$25 | No |
| Trimethoprim-Sulfamethoxazole | UTIs, bronchitis, skin infections | 3-14 days | Allergic reactions (sulfa), rash, low blood cell counts | $10-$30 | No |
| Fosfomycin | Uncomplicated UTIs (single dose) | 1 dose | Diarrhea, nausea | $30-$60 | No |
| Doxycycline | Sinus, Lyme, acne, pneumonia | 7-21 days | Sun sensitivity, stomach upset | $15-$40 | No |
| Amoxicillin-Clavulanate | Sinus, ear, lung infections | 7-10 days | Diarrhea, yeast infections, allergic reactions | $20-$50 | No |
When Cipro might still be the right choice
Just because there are safer options doesn’t mean Cipro has no place in treatment. Here are situations where it’s still necessary:
- You have a kidney infection (pyelonephritis) caused by a resistant strain
- You’re allergic to all other first-line antibiotics
- You have a severe prostate infection that didn’t respond to other drugs
- You were exposed to anthrax (Cipro is FDA-approved for this)
- Your culture shows the bacteria are sensitive to Cipro and resistant to all alternatives
In these cases, the risk of not treating the infection outweighs the risk of Cipro’s side effects. But even then, doctors should monitor you closely.
What to ask your doctor
If you’re handed a Cipro prescription, don’t just take it. Ask these questions:
- Is this infection likely to be caused by a bacteria that Cipro can treat?
- Are there safer, equally effective antibiotics I could take instead?
- Could this be a viral infection that doesn’t need antibiotics at all?
- What are the signs of serious side effects I should watch for?
- Can we do a urine or culture test first to confirm the bug and its sensitivity?
Doctors aren’t always aware of the latest guidelines. If you’ve had side effects from antibiotics before, or if you’re over 60, pregnant, diabetic, or have kidney problems - make sure they know.
What to do if you’ve already taken Cipro
If you finished your course and felt fine, great. But if you started having pain in your tendons, tingling in your hands or feet, sudden anxiety, or dizziness - don’t ignore it. These can show up days or even weeks after stopping the drug.
Stop taking Cipro immediately and contact your doctor. Report the symptoms to the FDA’s MedWatch program. You’re not overreacting - these side effects are real and documented.
Recovery can take months. Physical therapy helps with tendon issues. Some people need nerve specialists for neuropathy. Don’t wait for it to get worse.
Bottom line: Don’t assume Cipro is the best option
For most common infections - especially UTIs, sinus infections, or ear infections - Cipro is no longer the first choice. Safer, just-as-effective antibiotics exist. The real question isn’t whether Cipro works - it’s whether you need it at all.
Antibiotics should be used like a scalpel, not a hammer. Cipro is a powerful tool, but it comes with serious risks. Always ask: Is there a safer alternative? And if not - why not?
Is Cipro stronger than amoxicillin?
Cipro and amoxicillin work differently. Cipro kills a wider range of bacteria, including some that amoxicillin can’t touch - like Pseudomonas. But amoxicillin is safer and just as effective for common infections like ear infections, strep throat, and many UTIs. Strength isn’t the same as appropriateness.
Can I take Cipro if I’m allergic to penicillin?
Yes, Cipro is not related to penicillin, so a penicillin allergy doesn’t automatically mean you can’t take it. But that doesn’t mean you should. There are safer alternatives like nitrofurantoin or fosfomycin for UTIs, and doxycycline for respiratory infections. Always discuss your allergy history with your doctor.
How long does it take for Cipro to work?
Most people start feeling better within 24 to 48 hours. But you must finish the full course - even if you feel fine. Stopping early can lead to resistant bacteria. If you don’t improve after 3 days, contact your doctor. The infection might not be bacterial, or the bacteria may be resistant.
Is there a natural alternative to Cipro?
No. While some natural remedies like cranberry juice or garlic have mild antibacterial properties, they cannot replace antibiotics for serious infections. Relying on them instead of proven medicine can lead to sepsis, kidney damage, or death. Antibiotics are the only proven treatment for bacterial infections like UTIs, pneumonia, or prostatitis.
Can Cipro cause long-term damage?
Yes. The FDA has confirmed that fluoroquinolones like Cipro can cause long-term or permanent damage to tendons, nerves, muscles, and even the aorta. Symptoms like chronic pain, numbness, or mobility issues can appear months after taking the drug. If you’ve taken Cipro and now have unexplained symptoms, get evaluated by a specialist - don’t assume it’s aging or stress.
Why do some doctors still prescribe Cipro?
Some doctors still prescribe it out of habit, lack of updated training, or because they’re treating a complex infection where alternatives failed. Others may not be aware of the latest FDA warnings. Patient pressure also plays a role - if someone says, “My friend took Cipro and it worked,” doctors sometimes give in. Always ask for evidence-based options.
Next steps: What to do now
If you’re currently on Cipro:
- Don’t stop suddenly unless you have severe side effects - talk to your doctor first.
- Watch for tendon pain, numbness, dizziness, or mood changes.
- Drink plenty of water and avoid excessive sun exposure.
If you’ve been prescribed Cipro but haven’t started yet:
- Ask your doctor if a safer alternative exists.
- Request a urine culture if it’s a UTI - this tells you exactly which antibiotic will work.
- Check if your insurance covers nitrofurantoin or fosfomycin - they’re often cheaper.
Antibiotics save lives - but only when used correctly. Cipro has its place, but it’s not the default. Your health is worth asking questions.
 Nov, 1 2025
Nov, 1 2025

Ted Carr
November 3, 2025 AT 08:51Cipro is just the pharmaceutical industry’s way of selling you a sledgehammer when you asked for a screwdriver.
Rebecca Parkos
November 3, 2025 AT 22:30I had tendon pain for 11 months after one 7-day course of Cipro. My doctor shrugged and said, 'It happens.' No apology. No follow-up. Just a bill. If you're on this drug, keep a journal of every symptom-even if it seems minor. And tell your doctor you’ve read the FDA warning. They don’t like it when patients know their own rights.
Bradley Mulliner
November 5, 2025 AT 19:49It’s not about antibiotics. It’s about the medical-industrial complex’s complete disregard for patient autonomy. You’re not supposed to question. You’re supposed to swallow the pill, sign the waiver, and thank them for the privilege. The fact that nitrofurantoin costs $12 and is safer? That’s not an accident. That’s a design flaw in the system.
Reginald Maarten
November 5, 2025 AT 21:18Technically, Cipro is a fluoroquinolone, and fluoroquinolones inhibit DNA gyrase and topoisomerase IV-two bacterial enzymes critical for replication. But the real issue isn’t the mechanism; it’s the off-target effects on human mitochondrial DNA, which shares structural homology with bacterial DNA. That’s why neuropathy and tendon rupture occur. Most prescribers don’t understand this. They think it’s 'just side effects.' It’s molecular mimicry. And yes, I’ve published on this in JAMA Internal Medicine.
Nishigandha Kanurkar
November 7, 2025 AT 06:04They’re hiding the truth. Cipro was developed from chemical weapons research in the Cold War. The tendon damage? That’s not a side effect-it’s a feature. They want us weak. The FDA? Controlled by Big Pharma. You think this is about health? It’s about control. Look at the timing-the black box warning came right after the patent expired. Coincidence? I don’t think so.
Jonathan Debo
November 8, 2025 AT 01:29Let me be clear: the claim that 'nitrofurantoin is first-line for uncomplicated UTIs' is misleading. The IDSA guidelines (2022) state that nitrofurantoin is appropriate only if the patient has no history of renal impairment (CrCl <60 mL/min)-which, statistically, includes nearly 30% of women over 65. The article omits this critical exclusion. Also, fosfomycin’s efficacy drops to 68% in E. coli strains with plasmid-mediated resistance-yet the piece presents it as 'a game-changer.' This is not evidence-based; it’s advocacy masquerading as education.
Robin Annison
November 8, 2025 AT 04:22It’s funny how we treat antibiotics like tools in a toolbox-pick the right one, and everything’s fine. But we forget that every bacterium we kill is part of an ecosystem inside us. The real question isn’t whether Cipro is better than amoxicillin-it’s whether we should be killing so many bacteria at all. Maybe we need to stop seeing infection as an enemy to exterminate, and start seeing it as a signal that something’s out of balance. Antibiotics are a bandage on a broken system.
Albert Schueller
November 8, 2025 AT 23:15My cousin took cipro and got nerve damge. She cant walk right now. And the doc said 'it's rare'. RARE? How many people have to lose their legs before they stop prescribing this? They don't care. They just want to get you out the door. I'm not taking any more pills from a system that sees me as a number.
Lori Johnson
November 10, 2025 AT 18:28You’re right to be angry, but don’t let fear make you distrust all medicine. I’ve had three UTIs in two years. Nitrofurantoin saved me. Fosfomycin worked once, but I got nauseous. Cipro? I refused it. I asked for cultures. I got the right drug. It’s not about rejecting doctors-it’s about being a partner. And yes, I printed out the FDA warning and handed it to my GP. He actually thanked me.
Tatiana Mathis
November 11, 2025 AT 03:45There’s a quiet revolution happening in primary care, and it’s not about new drugs-it’s about slowing down. I’m a nurse practitioner, and I’ve started asking every patient: 'What’s your goal here?' For a UTI? To feel better. Not to 'kill every bug.' That’s why I prescribe nitrofurantoin, wait 24 hours to see if symptoms improve, and only escalate if needed. We used to rush to antibiotics because we were afraid of being sued. Now we’re afraid of harming people. That shift? It’s real. And it’s working. You’re not alone in this. There are doctors who care. They’re just not the ones yelling the loudest.
Michelle Lyons
November 11, 2025 AT 15:38They’re putting Cipro in the water. You think this is a coincidence? Fluoroquinolones are in the rivers now. Fish are developing resistance. That’s why your skin breaks out. That’s why your joints ache. The government knows. They’re testing it on us. You think the FDA is protecting you? They’re protecting profits. I’ve seen the documents. They’ve known since 1998.
Rahul hossain
November 12, 2025 AT 22:15When I was in Delhi last year, I had a fever-doctor gave me cipro. I felt better in two days. But I didn’t know the risks. Now I read everything. In India, we don’t have the luxury of choice. Antibiotics are sold over the counter. No culture. No consultation. We swallow what’s handed to us. But here, in the West, you have access to information. Use it. Don’t just accept. Ask. Push back. Even if they roll their eyes. Your body isn’t a vending machine.